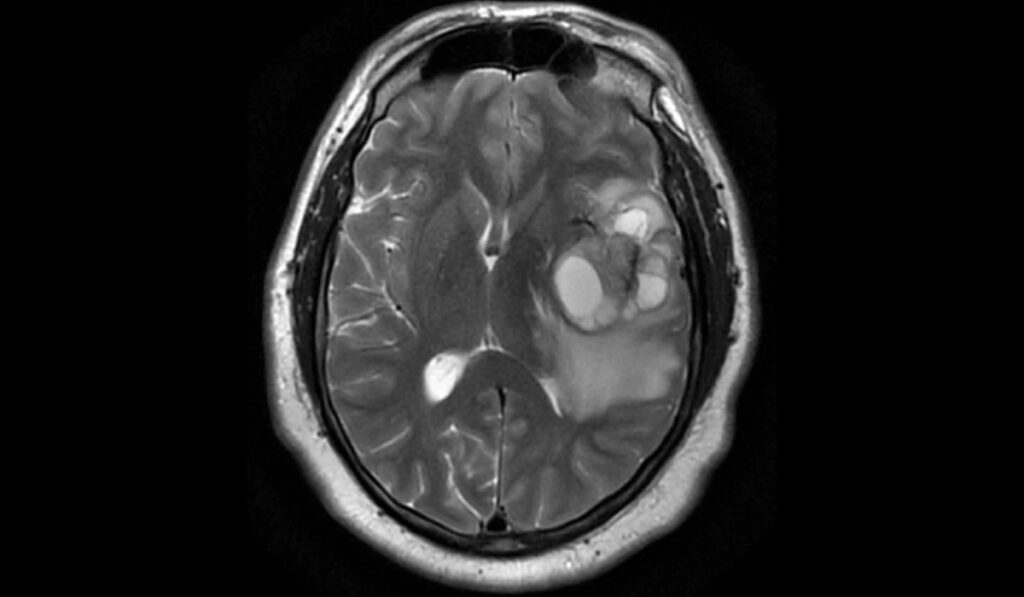
Gliomas, which include glioblastomas and astrocytomas, are among the most aggressive types of primary brain tumors. Patients live only about 15 months, on average, after diagnosis of glioblastoma.
With current systemic chemotherapy and immunotherapy essentially impotent in altering the disease course, investigators at Vanderbilt University Medical Center are now probing how to impact tumor growth by altering epigenetic characteristics.
The team recently completed an investigation of DNA methylation levels of tumor epigenomes that was launched to test whether glioblastomas are more hypomethylated than slower-growing brain tumors, like oligodendrogliomas. The phase I results suggest that hypermethylating these tumors can change the epigenome, modify gene expression, and slow tumor growth.
If confirmed, priming tumors with an epigenome-modifier, like high-dose L-methylfolate, might improve the efficacy of immunotherapy in this intractable disease.
The work was conducted by Vanderbilt colleagues Stephen Clark, M.D., an assistant professor of neurology; Paul L. Moots, M.D., chief of neuro-oncology; Bret C. Mobley, M.D., director of the Division of Neuropathology; Thomas G. Stewart, Ph.D., assistant professor of biostatistics; and other collaborators. It was published in Cancer Research Communications in January of 2022.
“This study demonstrates that it is possible to modify the epigenome as a new treatment for glioblastoma,” Moots said.
He cautions that larger studies are needed to prove whether this kind of approach is effective.
Manipulating Methylation
While multiple mechanistic changes impact the development and growth of a glioma, the researchers focused on the critical cycle of DNA epigenomic methylation and demethylation. Typically, a gene is turned off when it is methylated, and turned on when it is demethylated.
“We believe that when a glioma genome loses methylation, the chromosomes begin to unravel and genes become abnormally active, leading to tumor growth,” Mobley said.
In a xenograft-induced glioma rodent model, folate increased global DNA methylation and reduced tumor size. Mobley says there is also encouraging evidence in humans that DNA hypermethylation is associated with improved survival in individuals with low-grade gliomas.
“This study demonstrates that it is possible to modify the epigenome as a new treatment for glioblastoma.”
“We set out to determine whether we could influence DNA methylation in glioblastoma,” Mobley said. “Specifically, we investigated whether the methylome can be reprogrammed to reverse the hypomethylation, and we want to know how this impacts survival.”
Equivocal Patient Outcomes
To answer these questions, the researchers tested the impact of high-dose L-methylfolate on recurrent high-grade gliomas confirmed to be isocitrate dehydrogenase (IDH) wildtype. Fourteen adult patients with recurrent tumors were enrolled, 13 with glioblastoma, one with anaplastic astrocytoma. Participants were given L-methylfolate in ranges of 15, 30, 60 or 90 milligrams daily.
To enable patients to derive possible benefits from a chemotherapy regimen, they were also given standard doses of temozolomide and bevacizumab during the trial period. Outcomes were compared with those of a retrospective control group of 50 patients who were on bevacizumab alone.
“Knowing we can alter the brain tumor epigenome is exciting news in a cancer where no significant improvements in patient treatment or outcome have recently been made.”
Survival of the study participants was 9.5 months versus 8.6 months in the controls. These differences did not reach statistical significance but, the authors note, the spectrum of outcomes was broad.
Influencing the poor survival end of the spectrum was the fact that most of these patients were well into the disease state when they began the treatment. On the other end, survival rates for some patients met the standard of long survival for this disease; six patients lived more than 650 days after treatment began and one patient lived 1,080 days.
Reprogramming the Methylome
A second part of the study sought to determine whether the treatment had reprogrammed the methylome. To find out, they compared patients’ initial tumor specimens to their autopsy specimens. Indeed, tumors from patients treated with L-methylfolate showed increased DNA methylation.
“The small size of this study didn’t allow us to determine if there could be an impact of this treatment on survival, but we were able to learn that glioma cancer cells can be ‘reprogrammed’ to DNA methylation states that may change tumor behavior,” Mobley said.
“Just moving the needle, knowing we can alter the brain tumor epigenome is exciting news in a cancer where no significant improvements in patient treatment or outcome have recently been made.”
Perhaps one future application of methylome reprogramming will be to use this intervention together with immunotherapy treatment for glioma. If tumors are primed, or pretreated, with an epigenetic modulator, the researchers theorize it could change gene expression and lead to new proteins being expressed on the surface of tumor cells. These new proteins could potentially serve as targets for the immune system to find and attack.