A robotically enhanced-view totally extra-peritoneal (eTEP) technique, newly applied to ventral hernia repair, is proving its mettle among surgeons experienced in robotic assistance technologies. Leading the pack is Joseph Broucek, M.D., who has performed scores of eTEP procedures and trained many others across the country in the technique.
Broucek, an assistant professor of surgery at Vanderbilt University Medical Center, is also working to put hard numbers on the costs and benefits of this procedure in comparison to open surgery, previously considered the gold standard. Studies to date have established that the durability of repair is equivalent, and that robotic procedures have the edge on hospital length of stay (LOS) and wound infection rate. Still missing until now has been data that paints a broad picture of the value for the patient and hospital across the course of hospitalization.
Broucek and Vanderbilt colleagues Joel F. Bradley, III, M.D., Meredith C. Duke, M.D., and Richard A. Pierce, M.D., are addressing these questions through reports on the first 25 patients to undergo the robotic eTEP procedure at Vanderbilt. They are comparing these to data from the Abdominal Core Health Quality Collaborative and from existing literature on open and robotic retromuscular ventral hernia repair across multiple study sites in the United States.
To date, their findings affirm previously demonstrated benefits, as well as a lower need for narcotic pain medication.
“At a big hospital like Vanderbilt, where we run at over 100 percent capacity. Shorter LOS allows us to free up beds for other critical care patients who need to be transferred in,” Broucek said. “This translates into value for both patients and the hospital system.”
eTEP Procedure Highlights
Broucek says the eTEP technique, originally developed for inguinal hernias, reduces the invasiveness of most hernia repairs and is solving some of the persistent suturing problems that may occur in both open and laparoscopic surgeries.
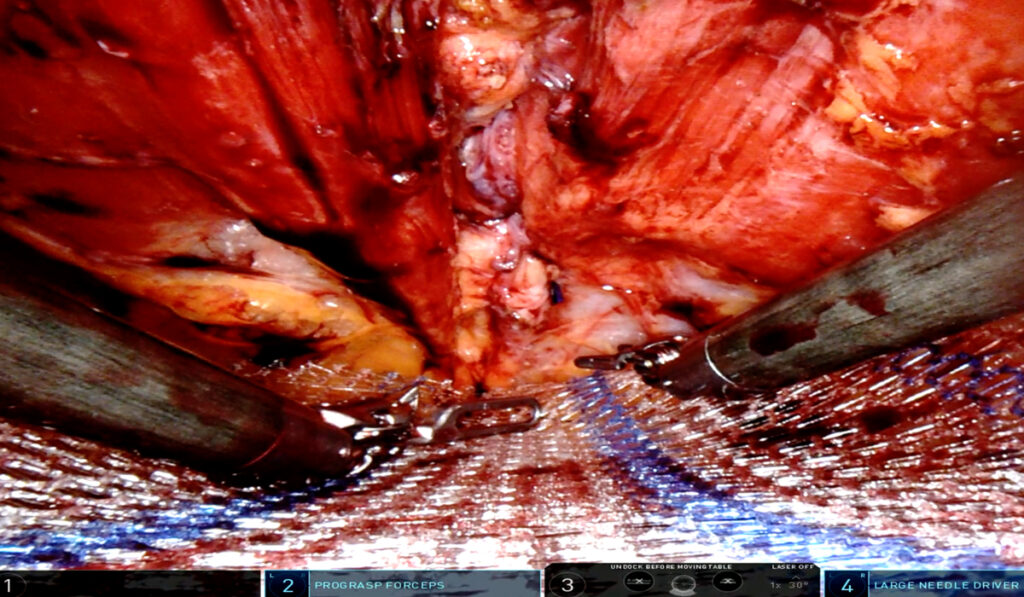
“With eTEP, we are exactly reproducing the Rives-Stoppa ventral repair, which is the current open-approach gold standard of hernia repair,” Broucek said. “We recreate this robotically, but we work between the layers of the muscle and the inner lining of the abdomen instead of going in fully transabdominally.”
The robotic procedure requires three or four small incisions, in contrast to the one large incision made in an open procedure, thus reducing pain scores and limiting opportunity for wound infection.
“The robotic procedures cost the hospital system about half of what the open procedures do.”
Key advantages over laparoscopic procedures are the 3D view and 360 degrees of motion in the robotic joint, plus suturing with ease in any direction. Broucek notes that the robot provides significant magnification to enhance fine dissection and electrocautery work and improve accuracy in other aspects of the surgery.
“It not only enhances the perioperative experience for patients but also for the surgeon, who is able to work in an upright seated position rather than standing for hours at a time,” he said.
Vanderbilt Outcomes Tallied
Today, Vanderbilt utilizes robotic approaches for about 60 to 80 percent of abdominal wall hernia repairs, Broucek says. Most are performed as outpatient or observation-based procedures.
Comparing the data from the first 25 eTEP repairs, Broucek found that surgical site infection and readmission rates were lower among the eTEP group compared with national data from other robotic approaches.
Wider differences appeared when comparing eTEP with open surgeries, with eTEP patients averaging a LOS of 2.6 days versus 4.7 days with open procedures. And fewer than 20 percent of these patients took narcotics after leaving the hospital.
“When we added in the lower complications and readmission rates with eTEP, savings across the entire ventral hernia program were substantial,” Broucek said. “Globally, the robotic procedures cost the hospital system about half of what the open procedures do. So, there is value not only to the patient but for the hospital system in embracing and investing in a robotic-based abdominal wall program.”
Sharing the Skill
“This is a very specific technique that is not yet widely adopted,” he said, although Broucek may be changing that fact by teaching cadaver-based courses in eTEP to experienced robotics surgeons throughout the country. Many will go on to introduce the technique at their own hospitals or academic centers, he said.
“We talk about pros and cons for their center, patient selection, and techniques to make a successful robotics program,” he said. “For many, I proctor or mentor them personally or virtually when they’re first starting to do these techniques at their hospital and am available to them as they put this into practice.”