New adjustable implant devices are broadening the options for spinal fusion surgery.
Pairing adaptive technology with a minimally invasive approach, Vanderbilt University Medical Center orthopaedic surgeon Raymond Gardocki, M.D., and others in the field are giving surgeons and their patients expanded options.
“It’s the best of both worlds,” Gardocki said, in speaking of the flexible interbody technology. “Traditionally, the smaller the corridor, the smaller the implant had to be.”
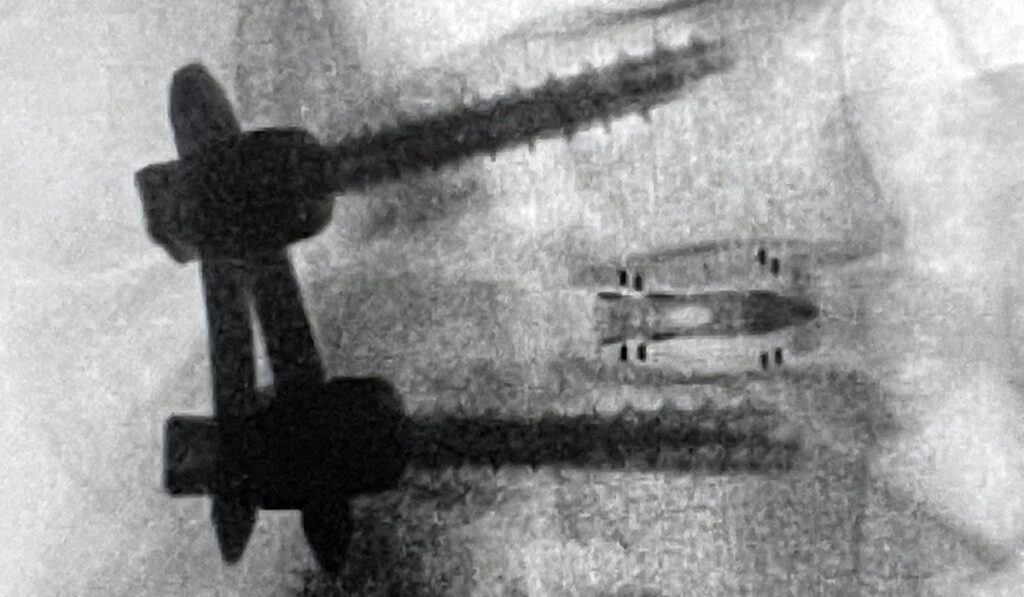
But the new adjustable device, which goes by the brand name Accelus FlareHawk7, can be implanted through smaller corridors – causing fewer disruptions of normal anatomy and minimizing nerve retraction . According to Gardocki, the device still fills the larger disc space and achieves high fusion rates with less subsidence.
As a note of disclosure, Gardocki was part of the development team and the first spine surgeon to endoscopically implant the customizable surgical device. Eventually, he hopes to realize financial rewards for the product, Gardocki said. He also helped design the endoscopic instrumentation for the newer, larger FlareHawk9.
Need for Sizing Options
“For decades, cages were all basically one size; you could change the height and length, but the width was always 11 millimeters,” Gardocki said.
“The idea is to create a platform where you have the flexibility to adapt to what the patient gives you – and do it on the fly.”
While larger cages generally provide better support and more leverage to recreate lordosis, a cage too large for the individual disc space presents issues.
“If you didn’t have 11 millimeters of width to be able to put that block in, you were going to hurt something,” Gardocki said.
To create sizing options, the adjustable device compresses to 7 millimeters in height and 7 millimeters in width and expands in increments to 12 millimeters tall and 11 millimeters wide. The second generation implement starts with a slightly larger insertion profile but can extend to 14 millimeters in both directions. Even larger devices will be added to the platform soon, Gardocki said.
Making the Tech Compatible Across Devices
The two-piece cage design includes a shell and a shim and is an offshoot of cardiac stent technology, Gardocki explained. All necessary inserters and disc preparation instruments are cross-platform compatible, with only the cannula delivery system varying to match device size.
Altogether, this built-in versatility enables surgeons to pick the implant and approach that best suits their patient’s unique anatomy. Gardocki said this is especially helpful when obstacles are encountered during surgery that may require a change of course, such as congenital spinal stenosis or dense scar tissue hindering nerve mobilization.
“The idea is to create a platform where you have the flexibility to adapt to what the patient gives you – and do it on the fly,” Gardocki said.
“You do a better job because you can actually see what you are doing.”
Visual Advantages
An endoscopic approach not only is minimally invasive, but the camera at the tip of the endoscope provides a valuable view of the disc space.
“Even in an open surgery, you can’t see into the disc from a posterior approach because, typically, you’re retracting between two nerves,” he said. “The hole in the disc space is a centimeter square or a little bit bigger, and you can’t really see into that, even with a microscope.”
This direct visualization gives surgeons a better perspective while removing the delicate cancellous bone cartilage. Residual cartilage can hinder disc fusion, while scratches or other bone defects can lead to stress risers and subsidence.
“You do a better job because you can actually see what you are doing,” Gardocki said.
Benefits of Ultra-Minimally Invasive Surgery
Gardocki, a national leader in ultra-minimally invasive endoscopic spine surgery, conducts outpatient procedures for almost all one-level and two-level lumbar fusions, as well as lumbar discectomies and decompressions, and cervical discectomies and decompressions.
Among the many benefits of endoscopic outpatient surgery is reduction in pain, reduced opioid prescribing, and faster time to ambulation.
“It’s hard to explain how much less invasive it is,” he said. “Average hospital stays for a patient in the United States for one-level lumbar fusion is in the range of three to four days. And right now, we’re averaging a range of three to four hours.”
Looking ahead, he envisions indications for expandable lumbar fusion devices widening, just like their footprint.
“These devices have the ability to be used in other applications, not just for posterior lumbar interbody fusion and transforaminal lumbar interbody fusion, but also with a lateral approach to the spine and an oblique anterior approach to the spine.”