Prescribing potentially inappropriate medications (PIMs) to older adults upon discharge from the ED is associated with a host of adverse events when compared with prescribing known safe medications or no new medications.
Among the concerns with PIMs are higher fall risks, negative drug-drug interactions, increases in repeat ED visits and higher hospital admission rates.
High-dose non-steroidal anti-inflammatory drugs (NSAIDs), sedatives, and anticholinergics top the most-prescribed medications on the Beers Criteria – the American Geriatric Society’s guide on PIMs for older adults.
In 2011, a group spearheaded by the Emory University Department of Medicine, and soon joined by Vanderbilt University Medical Center, worked with their respective Veterans Affairs (VA) hospital affiliates to tackle the persistently high rate of PIM prescribing (around 11 percent) among older veterans upon ED discharge.
James (Jim) Powers, M.D., a geriatrician and professor at Vanderbilt, has been a central player in this effort, which has grown to encompass 12 academic medical center-VA partnerships since its inception.
The goal of this initiative, Enhancing Quality of Prescribing Practices for Older Veterans Discharged from the Emergency Department (EQUiPPED), is to develop a model for ED education on prescribing for geriatric patients.
“It took awhile for us to arrive at a formula that worked in lowering rates of PIM prescribing, but once we did, our group saw dramatic improvements. Most importantly, the low prescribing levels have been sustained over time,” Powers said.
The Beers Criteria
In any given month, over 90 percent of adults 65 years or older use at least one prescription medication and over 66 percent use three or more, according to the American Geriatrics Society. Many of them take at least one inappropriate medication. Most older adults discharged from the ED will be prescribed at least one new drug, Powers adds.
The Beers Criteria were created to help providers make the most judicious decisions by listing medications known to increase hazards for older adults as a whole. It also lists safer alternatives (or dosages) where they exist. The list currently includes 56 PIMs, categorized by organ system, therapeutic category, disease state, drug-drug interactions and dosing selection.
“The prescriber is on the frontlines, and sometimes they do have to use some of these medicines. The Beers list is very clear that these are never flat-out recommendations, but rather ‘proceed with caution’ recommendations,” Powers said.
‘A Reasonable Floor’
The VA hospitals participating in EQUiPPED are all Geriatric Research, Education, and Clinical Centers (GRECCs), VA geriatric Centers of Excellence focused on aging. Powers says 10 to 15 percent of the medicines being prescribed at these centers prior to intervention meet Beers Criteria; the initiative’s goal is to push this to five percent at each facility.
“This seems to be a reasonable floor, beyond which it doesn’t make sense to push.”
The site teams use core interventions of education, informatics-based EHR clinical decision support, and individual provider feedback to influence prescribing behaviors.
“Once we started with the individual provider feedback, PIMs prescribing dropped two or three times and then was sustained.”
EQUiPPED Slashes PIMs Prescriptions
Sustainability was vital to establish. The project leaders compared the number of PIMs prescribed to ED-discharged veterans for at least six months prior to the first EQUiPPED intervention at each site and for at least 12 months following the final EQUiPPED intervention.
The first four of the urban VA sites to adopt the EQUiPPED model significantly cut their PIMs prescribing from 11.9 to 5.1 percent, from 8.2 to 4.5 percent, from 8.9 to 6.1 percent and from 7.4 to 5.7 percent.
The top five most frequently prescribed PIMs were diphenhydramine, hydroxyzine, skeletal muscle relaxants, chronic NSAIDs and promethazine, according to additional results published in the Journal of the American Geriatrics Society.
“The proportion of prescriptions decreased for all of these except hydroxyzine and diphenhydramine, and the greatest decrease occurred in muscle relaxants, with a 60 percent relative reduction,” the authors wrote.
“It took a few months to see results,” Powers said. “Once we started with the individual provider feedback, PIMs prescribing dropped two or three times and then was sustained around our goal of about five percent after six months to a year.”
At the patient level, about three percent of patients took a Beers Criteria medication and about one percent took two and sometimes more of the listed drugs, Powers says.
The Magic Formula
Powers says that testing the power of the three interventions – provider education, reprioritizing order sets in the EHR, and individual feedback – was instructive in itself.
“First, we had geriatricians giving lectures to ED providers and residents, but we saw very little behavioral change from that,” Powers said. “Then we offered up an easy way to prescribe safer alternatives to PIMs through the EHRs and it barely pushed the needle at all.”
Finally, they had monthly feedback from a graphic showing their PIMs prescribing level sent to them through email.
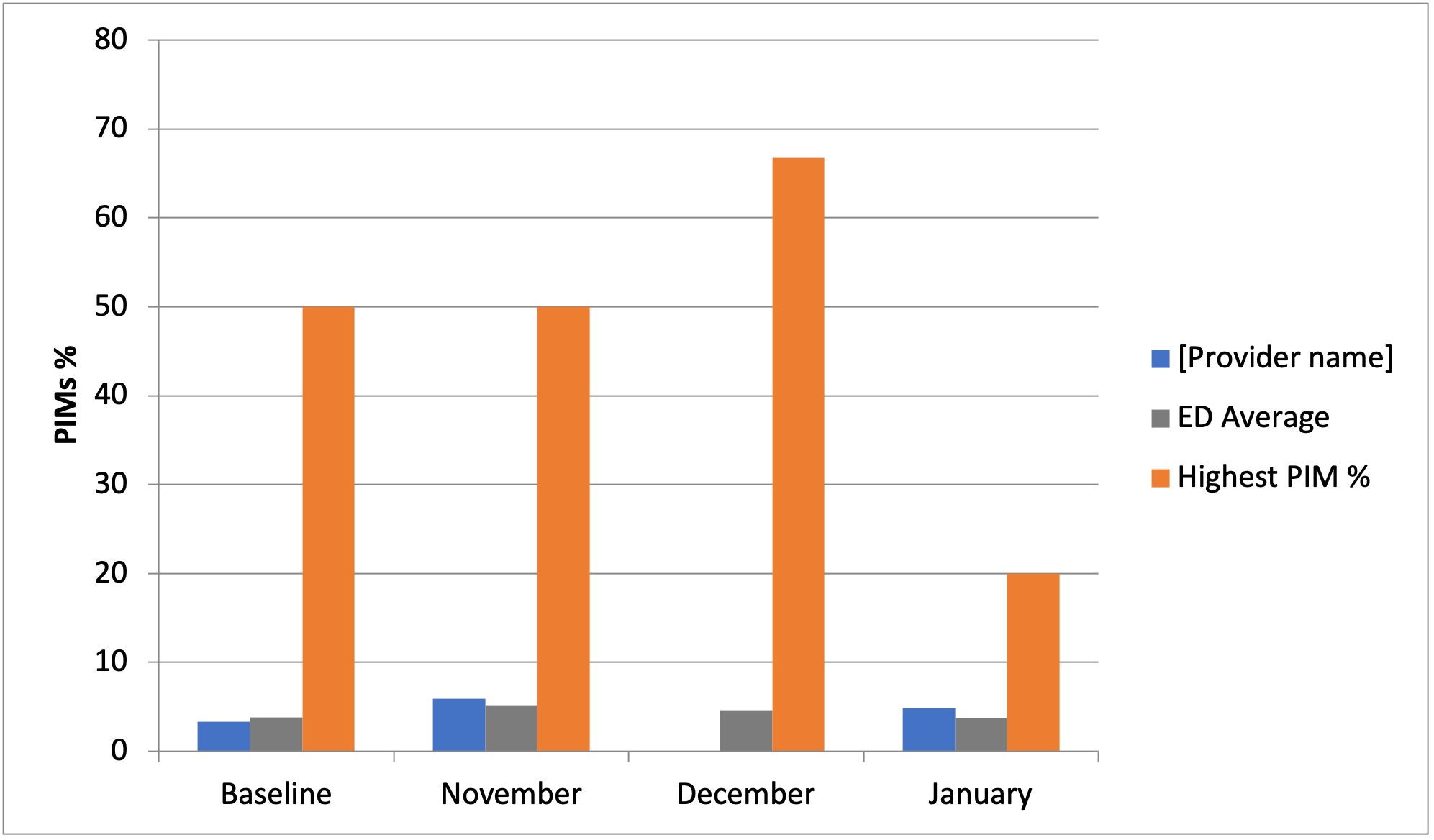
“This comparison approach worked some magic, perhaps because physicians generally don’t want to be practicing on the tail ends of the bell curve, and prefer, when possible, to be leading the pack in best practices,” Powers said.