Today’s data analytics have the capacity to inform best practices in real time, with laser-like focus. This leaves little room to justify wide variances in perioperative practice. The growing use of enhanced recovery pathways with standardized protocols reflects this understanding.
Vanderbilt University Medical Center has been adopting enhanced recovery pathways across several specialties, including colorectal, orthopaedics, urology and general surgery to continually improve patient experience. Lauren Prescott, M.D., an assistant professor of gynecologic oncology at Vanderbilt, leads the enhanced recovery effort for the Department of Obstetrics and Gynecology.
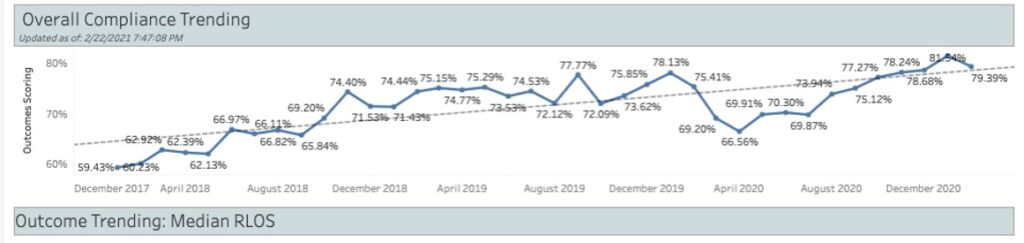
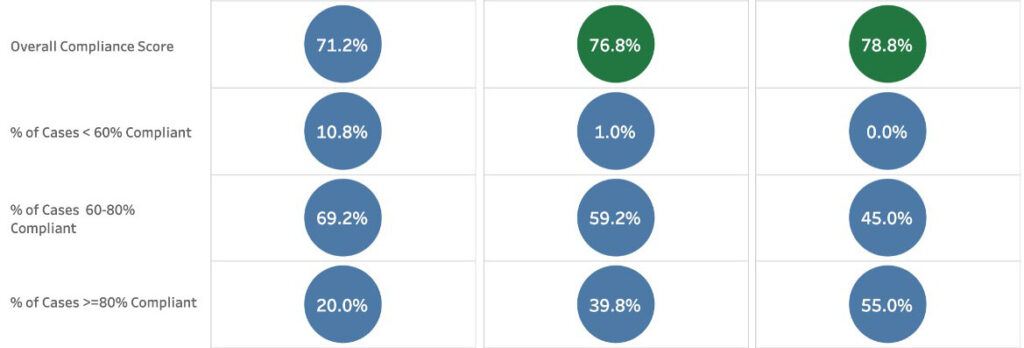
Since inception of the initiative in 2018, protocol compliance has increased significantly for surgeries in this pathway. Last year, Vanderbilt’s enterprise analytics group began providing Tableau software and other analytics programs to enable a real-time view of cases.
“Now, we see the timeline, the components of protocol, and complications within 30 days of surgery,” Prescott said. “This enables us to easily track protocol compliance at all stages – within 48 hours of surgery – and to measure outcomes.”
Designing and Refining the Pathway
The gynecology enhanced recovery team was tasked with consolidating best practices for elective hysterectomy, exploratory laparotomy, open oncologic surgery, and complex reconstructive pelvic surgery.
“There was significant variation in what medications were used depending on who your anesthesiologist and surgeon were, and patients were in the hospital varying amounts of time,” Prescott said. “The question was, how much of this was driven by patient differences and how much was due to non-standardized hospital practices?”
To answer this, the team developed a perioperative protocol, with a focus on improving patient preoperative education, standardizing preoperative medications, decreasing intraoperative and postoperative narcotics, and emphasizing early and frequent ambulation.
“The question was, how much of this was driven by patient differences and how much was due to non-standardized hospital practices?”
Prescott’s team meets regularly to review the compliance metrics, determine if benchmark goals are being met and develop quality improvement projects. This review includes evaluating each component of the protocol, including patient and provider compliance, to see how it is impacting outcomes.
A Real-time, Visual Synopsis
The team originally tracked data by manually entering compliance and 30-day perioperative outcomes into a REDCap database. However, this was time intensive, and compliance and outcome data were not accessible for months after entry.
The use of a digital analytics platform like Tableau enables a real-time review of the effectiveness of scores of perioperative practices. These include preoperative patient counseling about the surgery and anesthetic management, use of anti-bacterial wipes to avoid infection, administration of anti-nausea medications, maintenance of patient normothermia, regulation of glucose levels, and postoperative ambulation, eating, and catheter removal.
“These new resources were a game changer, enabling detailed analysis of compliance and outcomes,” Prescott said. “Combined with our REDCap database, we can now see where there are systemic issues and where we are not in compliance with our protocol. We can also test practices in a controlled, systematic way.”
Implementing Changes
The team uses Tableau’s quick and comprehensive data aggregation to drive small and large protocol changes, such as replacing epidurals with transversus abdominis plane (TAP) and rectus sheath blocks for all laparotomy patients. “We saw that epidurals were leading to more postoperative complications like hypotension, urinary retention and longer hospital stays,” Prescott said.
It is also driving simple changes like adding whiteboards with checkboxes in patients’ rooms as a visual reminder to get up four times a day. “Without the enhanced recovery pathway, we would not have known exactly where we were on ambulation compliance,” Prescott said.
“We saw that epidurals were leading to more postoperative complications like hypotension, urinary retention and longer hospital stays.”
Still, aligning physicians’ practices is not without challenges. A provider who has great outcomes with practices outside the protocol has an argument for not changing. “Sometimes we have to pick from two or more solid practices,” Prescott said. “What we do know is that universal adherence to one protocol is the only way that over time we can test the protocol and identify what we need to abandon and what new processes we should adopt.”