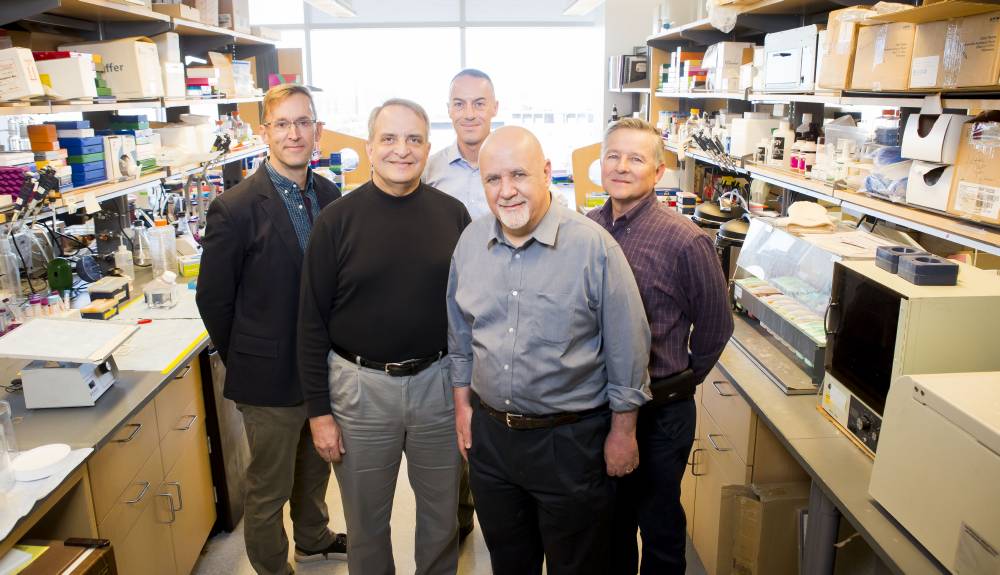
PediCODE, a research consortium on congenital diarrhea and enteropathy, is working under a five-year $9.4 million grant to characterize the clinical and pathophysiological features of congenital diarrhea in infants, identify unknown gene mutations, and develop a clinical database and biorepository of disease-specific cells and tissues.
Monroe Carell Jr. Children’s Hospital at Vanderbilt, the University of California Los Angeles Department of Pediatrics, the Hospital for Sick Children in Toronto, and Boston Children’s Hospital are collaborating in the research, funded by the National Institute of Diabetes and Digestive and Kidney Diseases.
“We estimate that about 50 percent of congenital diarrhea disorders do not have an identified gene. Our major goal over the next five years is to make that number much smaller,” said James Goldenring, M.D., Paul W. Sanger Professor of Experiential Surgery at Monroe Carell Jr. Children’s Hospital, and Vanderbilt’s principal site investigator. For previously characterized genes, the researchers plan to study mechanisms impacted by mutations.
PediCODE’s International Goals
Since its inception in 2016, PediCODE has grown to become a resource for multiple centers in fielding consults, both nationally and internationally, from the U.S. to the Middle East, Latin America and Europe.
“We are developing a clinical database and biorepository of disease-specific cells, tissues and other primary patient materials,” said Sari Acra, M.D., division chief of pediatric gastroenterology, hepatology and nutrition, and a co-investigator on the study. “We anticipate that these efforts we will help us identify novel genes implicated in the disease, while we establish a unique resource enabling mechanistic studies on its causes.”
“About 50 percent of congenital diarrhea disorders do not have an identified gene. Our major goal over the next five years is to make that number much smaller.”
A Lifetime of Daily Dependency
Congenital diarrhea is rare, and in most cases, there is currently no cure. The underlying etiology is often a conundrum to the treating physician, and can lead to delayed diagnosis, misdiagnosis or inappropriate therapeutic strategies. “By the time the cause is diagnosed, the baby may already be in a downward spiral,” Acra said.
The disease threatens dehydration, electrolyte imbalances and malnutrition, leading to failure to thrive, and in some cases, death. Affected children typically face a lifetime of total parenteral nutrition.
Small bowel transplant is an option of last resort, but carries significant infection and rejection risks. For these reasons, Acra says it is reserved for cases where diarrhea is poorly controlled or parenteral access is limited by vein thrombosis from repeated feedings.
Targeting Gene Mutations
Congenital diarrhea is often idiopathic, though trafficking barriers caused by genetic mutations appear to be the constant. Much of the team’s future work will focus on analyzing these genes. “When you do a genetic screen on a child, you’ll always see some mutations, but which ones fit the pathophysiology of the child’s diarrhea is the puzzle that we’re trying to figure out,” Acra said.
“We need to first understand what’s functionally wrong with the cells involved and then look for adaptive or curative solutions,” Acra said. Through preclinical models, Goldenring, Acra and their collaborators have already identified ion transport deficits that commonly underlie the pathology of one of the known mutations, microvillus inclusion disease (MVID). They are now working on interventions.
The research involves collecting patient tissue samples and using whole exome sequencing to identify known or candidate mutations, producing a tissue histopathology atlas. Intestinal organoids are grown from patient samples to recapitulate the specific disease. This enables researchers to study the mechanisms behind congenital diarrhea, as well as ways to restore normal electrolyte and nutrient trafficking.
Future Therapies
The hope lies in finding therapies that either correct the defects or provide adaptive support to the patient. To foster this, the Vanderbilt team will use the organoid model to test potential drug or nutrient therapies.
“Acting as mini-guts, organoids provide a particularly useful template for intestinal pathologies. Since the cells involved are derived from the patient, we can readily test drugs on the organoids and quickly measure the impact,” Acra said.
“We need to first understand what’s functionally wrong with the cells involved and then look for adaptive or curative solutions.”
Acra cites cystic fibrosis research as an example of how identifying the mutation, the transport problem it caused, and a drug that corrects the nutrient delivery malfunction (in this case, chloride transport) dramatically changed the outlook for patients. “If we identify the congenital diarrhea mutations and the transport defects they create, we can find ourselves on a similar path,” he said.