The death rate from thyroid cancer is low, and with nodules present in over 50 percent of middle-aged or older adults, thyroid cancer screening — and treatment – warrants ongoing scrutiny to avoid unnecessary interventions.
Lindsay Bischoff, M.D., an associate professor of diabetes, endocrinology and metabolism, and medical director of the Thyroid Center at Vanderbilt-Ingram Cancer Center, says more thyroid nodules are showing up on today’s sophisticated scans to detect other conditions, but up to 95 percent are benign.
Even in the 5 percent that are malignant, treatment is becoming less aggressive. “The culture of thyroid cancer management has changed dramatically in the past five to 10 years,” Bischoff said. “This is a disease where treatment was once ‘one size fits all’ – a total thyroidectomy, radioiodine therapy and lifelong thyroid suppression hormone.”
Guidelines are changing in recognition that thyroid cancer is much more nuanced than once believed, she added, and management merits a more precision approach. “We’re recommending a lot less intervention in many cases.”
Guidelines for Surveillance
Bischoff serves on the American Thyroid Association committee that is now rewriting the thyroid cancer guidelines. “We will address active surveillance for the first time in guideline form,” she said. “We hope to get this next iteration out in one to two years.”
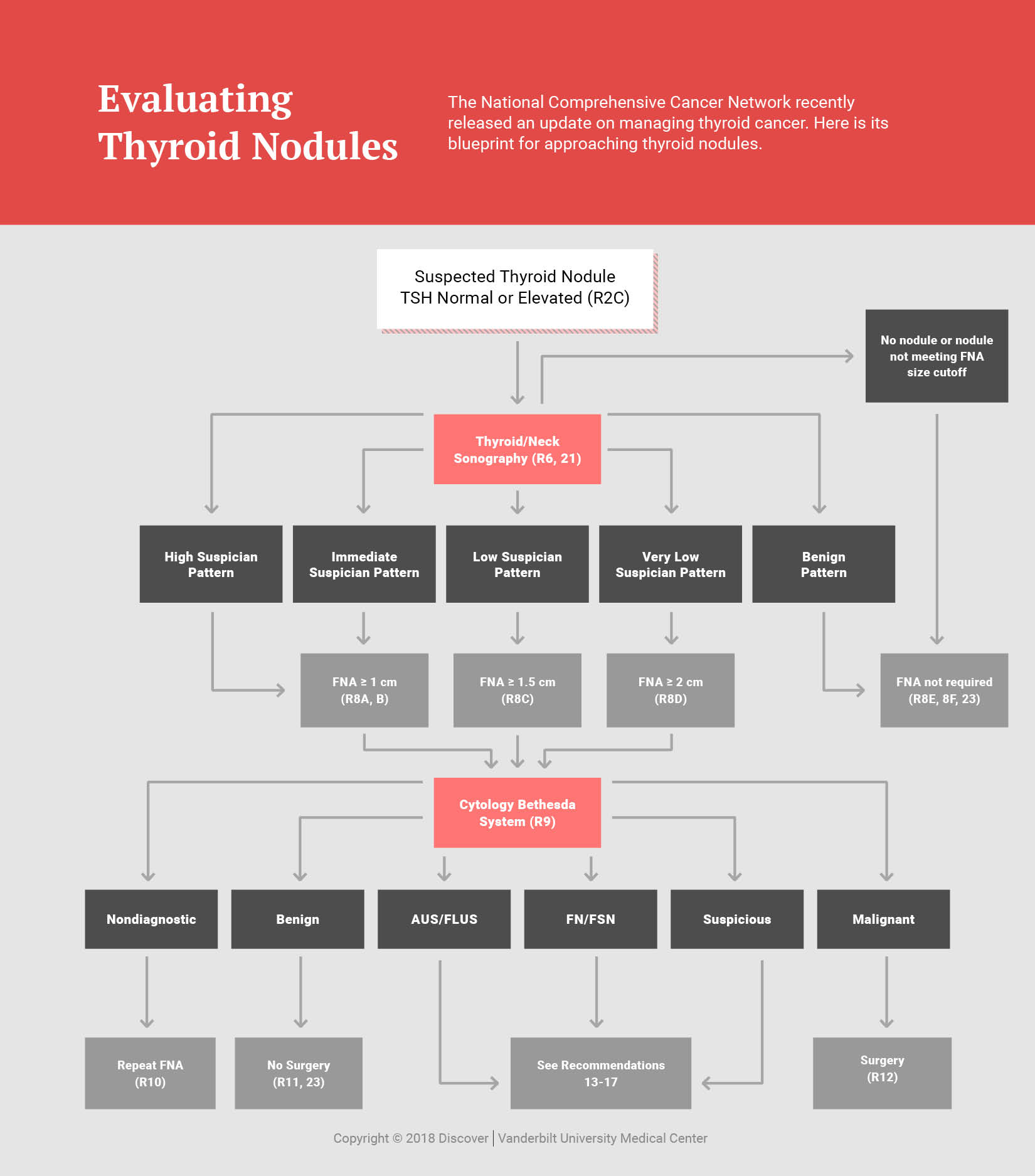
The gold standard for thyroid cancer diagnosis is still ultrasound evaluation of thyroid nodules and measurement of serum thyroid-stimulating hormone (TSH) levels to determine whether a fine needle aspiration biopsy is indicated.
“This is a disease where treatment was once ‘one size fits all’ – a total thyroidectomy, radioiodine therapy and lifelong thyroid suppression hormone.”
However, thyroid nodule evaluation is increasingly guided by a new tool called TI-RADS™ (Thyroid Imaging and Reporting Data System), developed by the American College of Radiology in 2017. The size cutoffs for biopsy are larger than the ATA system previously designated, resulting in fewer biopsies overall.
“TI-RADS has been shown to result in fewer biopsies with the same sensitivity for thyroid cancer as the ATA system,” Bischoff said.
Precision Cancer Therapy
Individualized, precision treatment takes several new changes into account – updates in the staging system, changes in the assessment of recurrence risk, and new tools for aggressive cancers.
At Vanderbilt today, thyroid cancer surgery is based on biopsy result and preoperative imaging of the thyroid gland and neck lymph nodes. If the thyroid gland does not have any nodules on the opposite side, there are no concerning lymph nodes, and the nodule is less than 4 cm, a lobectomy may avoid lifelong thyroid hormone replacement.
For non-aggressive types, Bischoff follows the updated tumor metastasis staging system, developed by the American Joint Committee on Cancer in 2018. This update reflects a new assessment of mortality rates, raising the age bands in which the (still low) risks of more rapid stage progression rise.
“Now we have more clarity on the high and low end. It is the intermediate risk patients for whom we are still trying to determine the benefit.”
Bischoff says that even more useful is the updated ATA-based assessment of risk for recurrence. These reflect evidence that patients with low risk for recurrence do not benefit from radioactive iodine therapy, while patients with high risk do.
“We used to say that anyone who had lymph node involvement got radioiodine,” Bischoff said. “Now we have more clarity on the high and low end. It is the intermediate risk patients for whom we are still trying to determine the benefit,” she said.
In the rare cases of aggressive thyroid cancer, Bischoff says that the chemotherapy options were traditionally quite limited. “Today, however, that is changing. Genetic testing is now expanding the options for targeted systemic therapy,” she said. “Debrafinib has improved response rates in cancers from BRAF mutations and entrektanib or larotrectonib are effective against tumors associated with NTRK mutations.”
Reassurance, with a Watchful Eye
With thyroid cancer’s 98 percent survival rate, Bischoff says the discussion is about recurrence risk – not the risk of a shortened lifespan. “However, patients understandably get nervous when they hear the ‘C’ word. It’s a difficult line for us to walk as physicians because there are some concerning cases,” she said. “We have a significant discussion with the patient to ensure they won’t have undue anxiety, and are sure to follow them carefully with blood tests and ultrasound surveillance.”
“In medicine we want to increase survival and decrease morbidity, but we shouldn’t be subjecting people to unnecessary surgery or therapies. Sometimes doing less is more appropriate than doing more.”