Retinoblastoma is the most common intraocular cancer in children. While more than nine out of 10 children in the United States are cured, the outlook is not as good if the cancer has spread outside the eye.
The retinoblastoma program at Monroe Carell Jr. Children’s Hospital at Vanderbilt integrates clinical care and research to offer a personalized, whole-child approach to retinoblastoma treatment.
“This is truly a collaborative effort between pediatric oncology, ophthalmology, radiation oncology, surgery, genetics and neurosurgery,” said Debra Friedman, M.D., director of pediatric hematology and oncology at Vanderbilt University Medical Center. “We support the child and their family throughout their treatment with nursing, child life, social work, psychology and nutrition services.”
For two decades intravenous chemoreduction (IVC) was the mainstay of retinoblastoma therapy, with the immunosuppressive treatments raising the risk of infection, need for transfusion and even subsequent cancers. As an alternative approach, Vanderbilt was one of the first centers nationally to adopt intra-arterial chemotherapy (IAC) that delivers chemotherapy into the ophthalmic artery through an endovascular microcatheter.
Efficacy without Toxicity
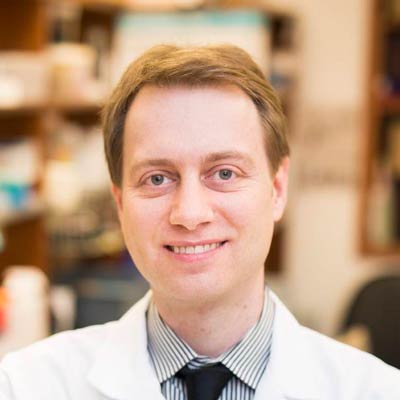
IVC, while effective, can be toxic for young patients, said Anthony Daniels, M.D., chief of the Division of Ocular Oncology and Pathology at the Vanderbilt Eye Institute.
“Retinoblastoma patients can be under a year old. Targeting the ocular tumor spares the rest of the child’s body from the long-term effects of chemotherapy. Additionally, in advanced intraocular retinoblastoma, intravenous chemoreduction success rates were under 35 percent. We knew there must be a better way.”
Daniels notes the increased efficacy of IAC is especially evident in eyes with more advanced disease, such as difficult-to-treat group D retinoblastoma. In a retrospective case study of Vanderbilt patients, Daniels, Friedman and colleagues reported IAC’s excellent treatment response in rare cavitary retinoblastoma tumors.
“We’re tracking visual, psychosocial, and learning outcomes, as well as family function. This will be instrumental in providing families with information about what retinoblastoma looks like down the road.”
In a subsequent study comparing IAC with IVC for retinoblastoma, the team reported globe salvage to be 100 percent for IAC versus 58 percent for IVC. Total unintended healthcare encounters, unplanned hospitalizations, episodes of low blood counts and transfusions were all lower with IAC.
“Since we began using these advanced therapies, we’ve successfully eradicated 100 percent of these tumors,” Daniels said.
Collaborative-Care Model
Daniels and Friedman see all retinoblastoma patients together. If a tumor is suspected, Daniels conducts an in-depth exam under anesthesia and an MRI to observe the tumor and optic nerve.
Immediately following the exam, the physicians sit down with the family to explain retinoblastoma and the available therapies. Together, they decide on appropriate therapy – the eye may need to be removed if there are high-risk features revealed on exam.
“Since we began using these advanced therapies, we’ve successfully eradicated 100 percent of these tumors.”
If the patient is to receive IAC, Friedman and Daniels together determine the dose, and the pediatric oncology team follows the patient for any systemic effects. If the eye is enucleated and found to have high-risk features on pathology, they administer systemic chemotherapy to prevent the risk of metastatic spread.
The oncologists also work with the hereditary cancer clinic at Vanderbilt-Ingram Cancer Center to conduct genetic testing and determine if patients have the heritable form of the disease.
“These patients are at risk for multiple tumors throughout their lifetimes; they’ll have to have long-term surveillance,” Friedman said. As patients move into adulthood, they are supported by Vanderbilt’s REACH for Survivorship Program.
Translational Research
Today, Daniels, Friedman and colleagues are studying the biology and genetics of retinoblastoma, focusing on development of new, molecularly targeted therapies.
Daniels’ team developed the first small animal model of IAC to test the efficacy, safety and toxicity of these compounds. They have identified several agents that are just as effective as currently used regimens, but without the associated ocular toxicities.
“My discoveries in the laboratory are geared toward bringing targeted and personalized therapy to these young patients,” Daniels said.
Friedman and Daniels lead Vanderbilt participation in multiple clinical trials, including an international multi-racial and ethnic consortium of retinoblastoma survivors, organized to study health outcomes and genotype–phenotype correlations of disease presentation. Begun in 2006, the NIH-funded study is currently following 600 participants.
“Quality of survivorship is so important,” Friedman said. “We’re tracking visual, psychosocial, and learning outcomes, as well as family function. This will be instrumental in providing families with information about what retinoblastoma looks like down the road.”