Abatacept, a drug typically prescribed for rheumatoid arthritis, may also be effective in treating immune checkpoint inhibitor (ICI)-associated myocarditis, according to a study recently published in Cancer Discovery.
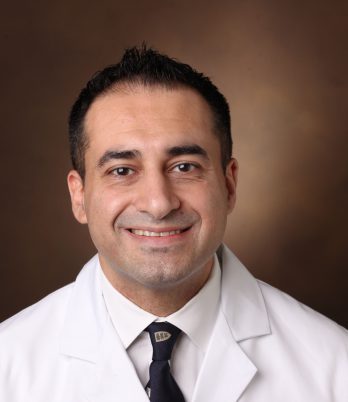
“We developed a preclinical model of ICI-associated myocarditis and used this model to provide mechanistic rationale for why abatacept, an already approved drug used for rheumatologic disease, may be a nice strategy to treat these patients,” said Javid Moslehi, M.D., director of cardio-oncology at Vanderbilt-Ingram Cancer Center and a corresponding author of the study along with James Allison, Ph.D., executive director of the Immunotherapy Platform at MD Anderson Cancer Center.
“We have a few examples of patients with ICI-myocarditis who responded to abatacept, but obviously we will need a larger trial to objectively assess,” Moslehi said.
Rare but Fatal Disease with Few Treatment Options
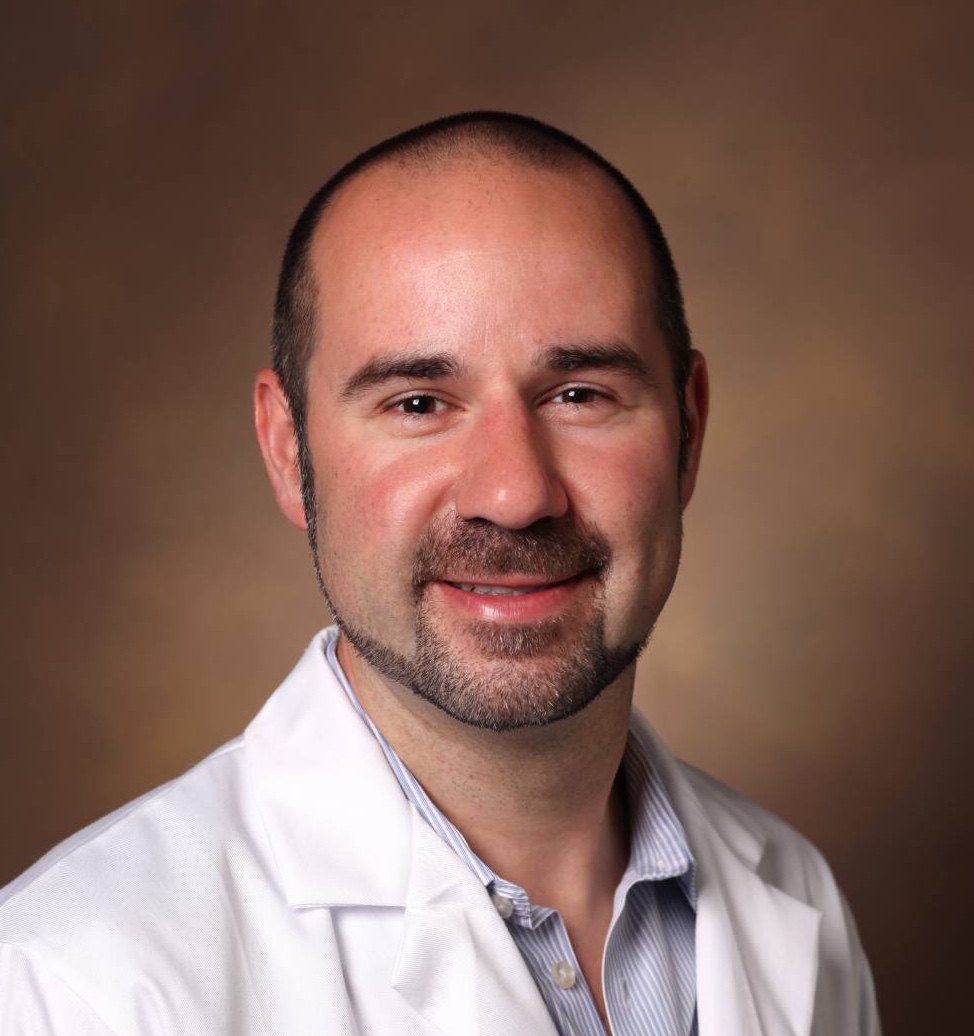
ICI-associated myocarditis – which is mechanistically distinct from myocarditis due to other causes – was initially described in 2016 by Moslehi and colleagues, including immuno-oncology experts Justin Balko, Ph.D., and Douglas Johnson, M.D., of Vanderbilt.
“Immune checkpoint inhibitors have revolutionized cancer treatment but are associated with immune-related side effects, such as myocarditis, which although infrequent, has up to a 50 percent mortality,” Moslehi said.
Currently, corticosteroids are the standard of care for cancer patients who develop myocarditis after treatment with ICIs, but Moslehi explains that they are not particularly effective.
“These are promising results, because we have few treatment options for the fulminant cases of ICI-myocarditis,” Moslehi said. “We give steroids as a way of suppressing the immune system, but ICI-associated myocarditis is often fatal despite corticosteroid treatment.”
“These are promising results, because we have few treatment options for the fulminant cases of ICI-myocarditis.”
Animal Model Brings New Understanding
In the new study, the researchers developed a preclinical mouse model that recapitulates the clinical course of ICI-associated myocarditis. Knowing that the major risk factor for ICI-associated myocarditis is combination ICI treatment with CTLA-4 and PD-1 therapy, the investigators designed the mouse model to lack a single copy of Ctla4 (encoding CTLA-4) and both copies of Pdcd1 (encoding PD-1).
Compound loss of the two genes led to premature death in 50 percent of the mice as a result of myocardial infiltration by T cells and macrophages as well as severe electrocardiographic abnormalities.
“We then used the animal model to identify drugs that reverse myocarditis,” Moslehi said. Restoration of CTLA-4 signaling via abatacept (an antibody-like therapy that restores CTLA-4 function) stopped disease progression and reduced deaths in the mouse model.
“This work gives us a unique opportunity to understand why this syndrome occurs, how to identify patients at risk for it, and maybe even how to prevent it from occurring in the first place.”
Treatment and Prevention
Clinically, Moslehi and colleagues have previously published a case report in which the use of abatacept successfully treated a severe corticosteroid-refractory ICI-myocarditis, and two additional cases of ICI-myocarditis treated with abatacept are reported in the new publication.
“As well as identifying a potential treatment, this work gives us a unique opportunity to understand why this syndrome occurs, how to identify patients at risk for it, and maybe even how to prevent it from occurring in the first place,” Balko said.