While infants and young children are far less susceptible to the ravages of COVID-19, the reason why has been puzzling. The strength of a young immune system alone doesn’t explain the low rates of infectious symptoms.
Children have lower levels of TMPRSS2, a serine protease gene that SARS-CoV-2 needs to invade airway epithelial cells in the lung. A new study, published in the Journal of Clinical Investigation, offers a compelling case that TMPRSS2 may be a key age-related determinant of SARS-CoV-2 infection.
“TMPRSS2 is unlikely to be the sole factor, but this work indicates that age-related changes in expression may significantly affect susceptibility to SARS-CoV-2,” said Bryce Schuler, M.D., a resident in pediatrics and medical genetics at Vanderbilt University Medical Center who worked with investigators Jennifer Sucre, M.D., an assistant professor of pediatrics, and Jonathan Kropski, M.D., on the study.
“TMPRSS2 is unlikely to be the sole factor, but this work indicates that age-related changes in expression may significantly affect susceptibility to SARS-CoV-2.”
Genetics of Lung Development
As members of the international Human Cell Atlas (HCA) Lung Biological Network, Kropski, Sucre and Schuler were well equipped to begin such a study. When the COVID-19 pandemic hit, they were completing a genetic data set on lung development from early life through adulthood.
“Our research has always focused on understanding lung development and how infant lungs differ from adult lungs in their vulnerability to injury,” Sucre said. “In this study we actually took the opposite approach and were able to see how the developing lung by its differences is protected from SARS-CoV-2 infection.”
The Vanderbilt COVID-19 Consortium Cohort, a multi-disciplinary effort to understand the risk factors of COVID-19 infection and illness, aided in the acquisition and analysis of human tissues.
Comparing the lungs of young mice and young people to adults using single-cell RNA-sequencing revealed two- to six-fold lower concentrations of TMPRSS2. “It is well-known that TMPRSS2 is a coreceptor for the coronavirus. What is special about our study is that we were able to show an age-related trajectory,” Schuler said.
Age-Related Expression
Coronaviruses depend on activation of host cell glycoproteins to enter. The Vanderbilt research team explored the developmental trajectories of ACE2 receptors, where the first step in the binding process occurs. They also studied TMPRSS2 and endosomal cysteine proteases furin and cathepsin B, coreceptors that populate the cell surface.
The new study describes an age-dependent, progressive increase in the proportion of TMPRSS2 among specific epithelial cell types in the respiratory tract. Of the genes tested, it had the most significant age-related trajectories.
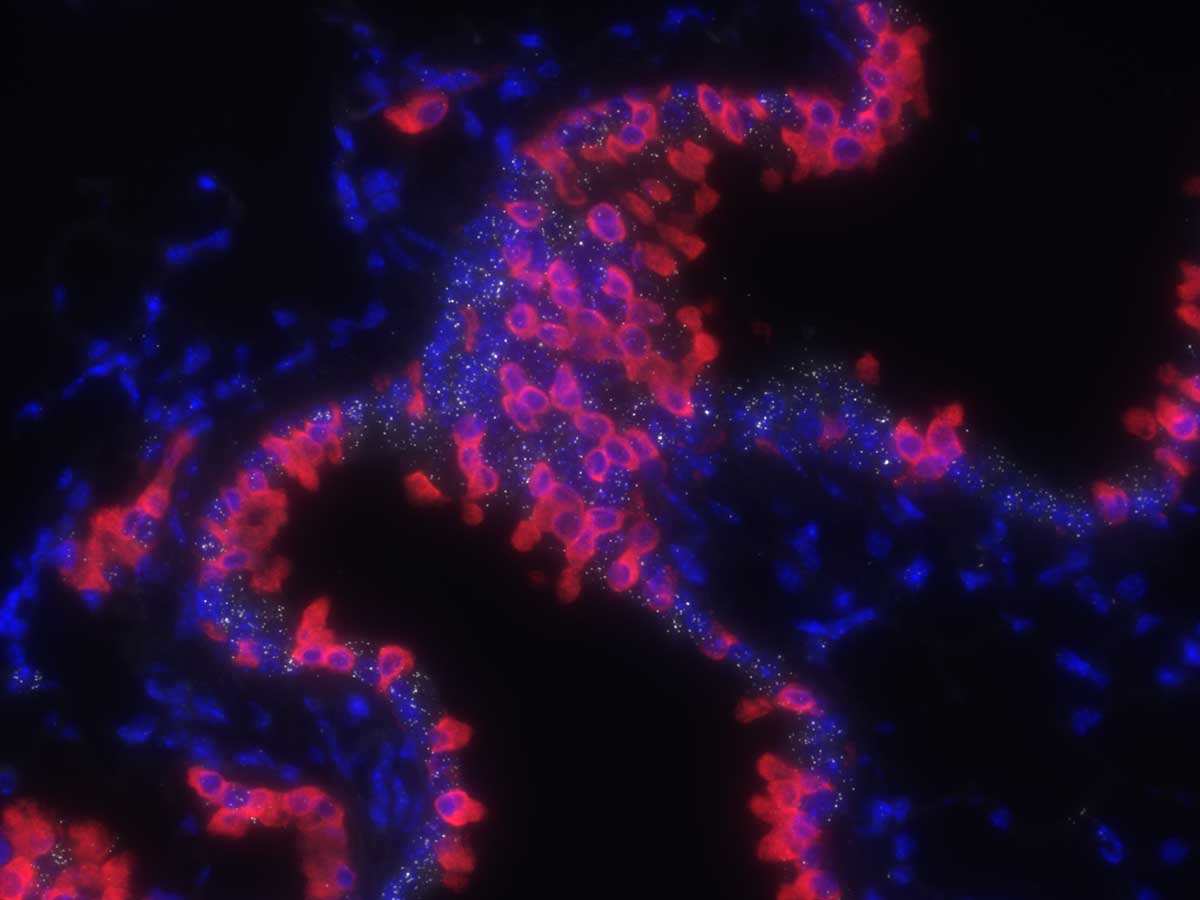
In both mouse and human tissue, the researchers found a greater concentration of TMPRSS2 expression in ciliated and type 1 alveolar cells, specifically. As they examined lung tissue from a patient who died of COVID-19, they found a high concentration of SARS-CoV-2 RNA in the same lung epithelial cell subtypes and co-localized with TMPRSS2.
Said Schuler, “This further supports the hypothesis that TMPRSS2 is a key player in mediating cellular infection by SARS-CoV-2.”
Implications for COVID-19 Therapy
“This study provides a potential biologic rationale for what we are observing clinically,” Sucre said. It may also explain why infants born to infected mothers tend to be spared. “Vertical transmission is incredibly rare, even when the placentas have lots of virus in them,” she added. “It really suggests that these babies are lacking key cellular machinery to let the virus in.”
“It really suggests that these babies are lacking key cellular machinery to let the virus in.”
Sucre points out that, fortunately, TMPRSS2 is a known agonist for prostate cancer. The antagonist camostat has been used to treat cancer patients for years. “So far, we have observed that these drugs effectively inhibit the virus in cultures. They could constitute a strategy to either prevent severe infection or serve a prophylactic role for people at high risk.”