For those ophthalmologists whose interests lie in public health, the exposure and tools needed may not be emphasized in residency training. One effort to provide cross-cultural public health training launched by the Vanderbilt Eye Institute (VEI) offers a reciprocal experience working with Georgetown Public Hospital Corporation (GPHC) in Guyana.
In a unique partnership, Vanderbilt residents will obtain real-world training in manual small incision cataract surgery (MSICS) and GPHC ophthalmologists will visit Vanderbilt for two-week observerships to learn from VEI faculty.
“Our residents will have the opportunity to see disease processes they would not see here in the U.S., learn a surgical skill, and share their knowledge,” said Laura Wayman, M.D., James H. Elliott Director and vice chair for education at VEI.
“Residents will have the opportunity to see disease processes they would not see here in the U.S., learn a surgical skill, and share their knowledge.”
The initiative is an example of a “twinning partnership,” defined by the World Health Organization as a collaborative partnership between individual institutions in developed countries and single or multiple institutions in less developed countries.
“In a modern eye institute, the training program has to incorporate a variety of experiences,” said Jennifer Lindsey, M.D., director of ophthalmology resident education at Vanderbilt. “We are excited to be able to offer this kind of real-world training to our residents.”
MSICS for Cataracts
While phacoemulsification is the preferred technique for cataract surgery in the developed world and tertiary centers, in developing countries MSICS is an established alternative. Numerous trials have proved that both techniques are safe and effective for rehabilitating the vision of cataract patients.
Most U.S. ophthalmology trainees perform primarily phacoemulsification when they are learning cataract surgical technique and may not gain proficiency in MSCIS.
“In many developing countries, ophthalmologists don’t have access to phaco equipment or may just have one older unit,” said Alexander de Castro-Abeger, M.D., now a first-year fellow and the first Vanderbilt resident to participate in the Guyana rotation. “Small-incision cataract surgery is almost half the cost of phacoemulsification and with less of a learning curve.”
Surgery in a Real-World Setting
The GPHC facility is a 600-bed, government-funded public hospital serving a population of more than 750,000 people. Medical students from the University of Guyana and Texila American University as well as nursing students from multiple nursing schools go there to train. Shailendra Sugrim, M.D., director of GPHC’s ophthalmology clinic, leads a small staff of ophthalmology-trained attendings, residents, nurses and optometrists.
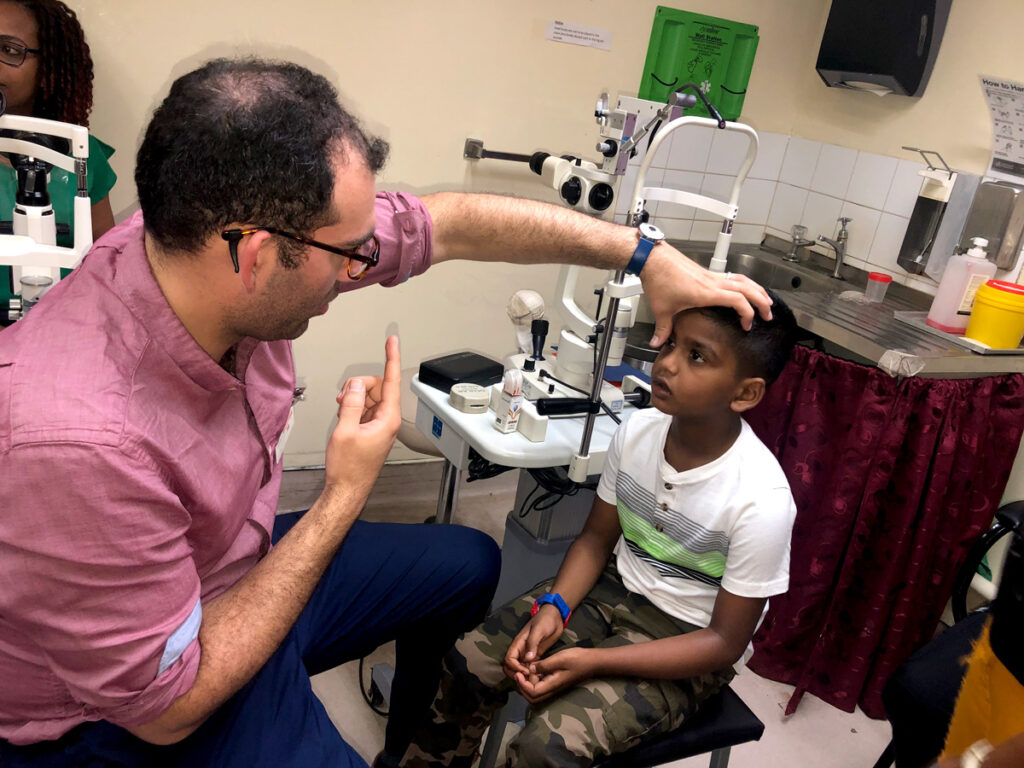
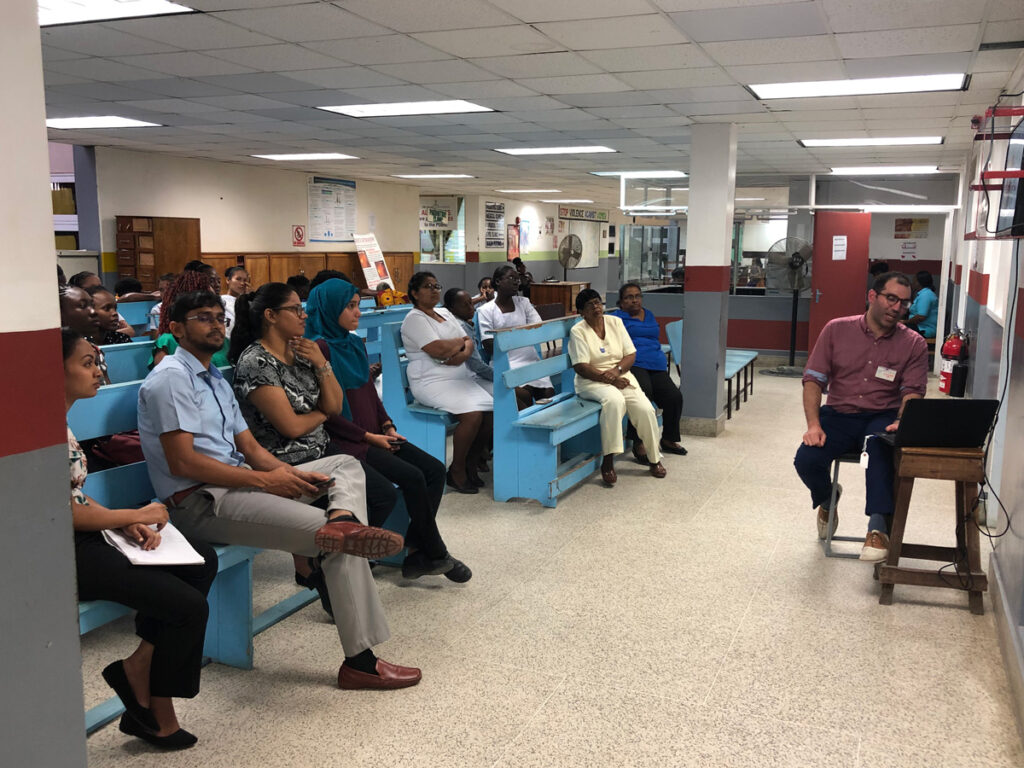
The first week of de Castro-Abeger’s rotation was spent evaluating patients in the triage clinic and determining treatment plans. He served as senior resident for ophthalmology interns and optometry students, led grand rounds, and presented lectures for trainees, ophthalmic nurses and staff. “This allowed me to leverage my knowledge and provided some great teaching experience,” he said.
Hands-on OR Experience
De Castro-Abeger also spent time observing Sugrim, who performs as many as 20 MSICS surgeries per half day in an operating room with two microscopes, one phaco machine and seven dedicated nurses. Small-incision surgery works in this context because it is shorter in duration than phaco, he explained. “When there’s a backlog of cataract patients, a surgeon using MSICS can be more productive.”
During the rotation, de Castro-Abeger completed 20 MSICS cases. In addition to overcoming a learning curve, he encountered various types of wounds requiring different incision lengths. “Each patient presented with a unique challenge,” he said. “I discussed possible approaches with the other attendings and was able to try different strategies.”
Lack of supplies and equipment is an issue at GPHC, says de Castro-Abeger. Antibiotic choices are limited, and the only steroid is dexamethasone. “Dr. Sugrim and the other ophthalmologists accomplish so much with so little. I brought back a list of supplies the next resident should take with them.”
Facilitating Collaboration
Orbis International is facilitating the program by providing linkages, training, research and travel grants. “Our partnership with GPHC provides exciting opportunities for trainees, VEI faculty and GPHC ophthalmologists,” Wayman said. “We are looking forward to strengthening this collaboration between VEI and our Guyanese colleagues.”