About 80 percent of people with heritable pulmonary arterial hypertension (PAH), a subtype of pulmonary hypertension, have a mutation in a gene called BMPR2. However, this single mutation is insufficient to explain the broad spectrum of symptoms, particularly in patients who present in infancy or early childhood.
T-Box genes, transcription factors active in embryogenesis, may help to fill the gap in understanding.
“Mutations in these genes appear to be a driver of the skeletal malformations, neurologic disorders, congenital heart defects and developmental disabilities we see in PAH diagnosed during infancy,” said Eric Austin, M.D., director of the Pediatric Pulmonary Hypertension Program at Monroe Carell Jr. Children’s Hospital at Vanderbilt.
Austin and his research collaborators recently described a complicated group of pediatric patients with mutations in the gene T-box transcription factor 4 (TBX4). Now, through a larger study, they are homing in on findings that PAH can present at various points before and after birth, and that earlier manifestation leads to PAH persistence for life.
Bringing New Insight into Syndromic Features
The researchers are testing whether children with deleterious heterozygous TBX4 mutations or TBX4-containing deletions have a unifying “TBX4 syndrome.” They are also exploring other genes that play a role in driving certain symptoms.
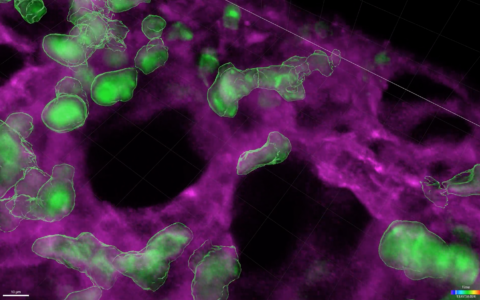
“We want to characterize these children and connect the dots between their lung/heart disease and the skeletal, neurodevelopmental and other abnormalities we see,” Austin said. “We are also exploring the molecular variations that result in TBX4-associated disease, especially as they relate to pulmonary vascular disease.”
“We want to characterize these children and connect the dots between their lung/heart disease and the skeletal, neurodevelopmental and other abnormalities we see.”
Austin and colleagues, including Rizwan Hamid, M.D., director of pediatric medical genetics and genomic medicine at Children’s Hospital, are studying the molecular mechanisms. They are also pursuing larger cohort- and population-based studies to better delineate genotype-phenotype correlations and determine future diagnostic and therapeutic strategies.
Expanding Clinical Evaluations
Austin says presentation variations among infants and children with severe PAH may prompt follow-up testing for TBX4, especially if the reasons for the comorbidities are uncertain.
“What is clear is that the prevalence of TBX4 syndrome among children with PAH is not trivial. Even prior to genetic testing, careful examination for skeletal abnormalities, airway diverticulosis, abnormal pulmonary function test results, or the presence of atrial septal and other congenital heart defects, should heighten suspicion of heritable TBX4-PAH,” Austin said.