In adults with congenital heart disease (ACHD) undergoing heart transplantation, donor oversizing is not associated with improved survival, according to research published earlier this year in The Journal of Thoracic and Cardiovascular Surgery.
“While there may be anecdotal cases that benefit from oversizing, our analysis of data from the UNOS (United Network of Organ Sharing) demonstrates that oversizing does not improve survival,” said Daniel Clark, M.D., first author on the study and a clinical cardiovascular fellow at Vanderbilt University Medical Center.
“While there may be anecdotal cases that benefit from oversizing, our analysis of data from the UNOS (United Network of Organ Sharing) demonstrates that oversizing does not improve survival.”
“In fact, donor oversizing may potentially worsen outcomes by increasing wait times for organs,” said Jonathan Menachem, M.D., a transplant cardiologist and director of Advanced Congenital Cardiac Therapies at Vanderbilt.
The Practice of Oversizing
Sizing hearts is a complex decision. Studies of the non-CHD population have consistently shown worse outcomes for undersized donors, particularly for those with pre-existing pulmonary hypertension.
Menachem says diagnosing pulmonary hypertension in ACHD can be challenging due to irregular anatomy and unequal blood flow to each lung. As a result, some centers have adopted a practice of empirically oversizing heart transplant donors for ACHD patients out of fear that there may be undiagnosed pulmonary hypertension that could lead to donor organ failure.
“The field of ACHD has grown rapidly and with that growth has come improvement in data collection and our ability to make evidence-based decisions and not those based on tradition,” Menachem said. “The issue with clinical decisions based on tradition is they can turn into standard of care when in fact they may not benefit patients.”
Effect of Sizing on Survival
For the study, researchers used UNOS data to complete a retrospective cohort analysis of ACHD patients who underwent a heart transplant in the U.S. between January 2000 and December 2015.
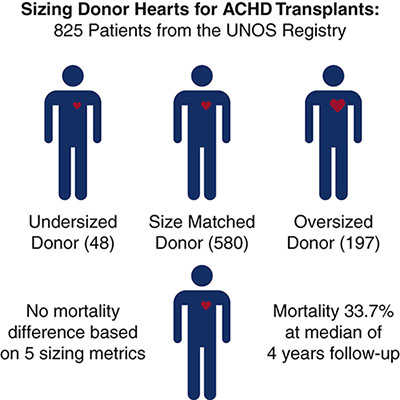
Predicted total heart mass was used as the representative donor sizing metric; of 825 patients, 48 were undersized, 580 were size matched, and 197 were oversized. Overall mortality at a median of four years of follow-up was 33.7 percent, with no mortality difference based on donor size matching.
Analysis of other donor sizing metrics, including height, weight, body mass index, and left ventricular mass also revealed no relationship between donor sizing and mortality.
Menachem says the results were surprising. “For years, experts in the field have empirically supported this idea of oversizing, and we are guilty of believing the myths.” Adding, “We are excited that [these] data may help break down some of the barriers that exist in getting ACHD patients transplanted.”
Metrics that were found to be associated with reduced survival include sex mismatch, preoperative renal dysfunction, and longer ischemic times.
“[These] data may help break down some of the barriers that exist in getting ACHD patients transplanted.”
A New Frontier
Due to the success of treating CHD in children, there is a growing population of adults with the disease. “As they age these patients develop heart failure, which is now the number one cause of death for ACHD patients. This has led to more patients requiring heart transplantation,” Menachem said.
“There’s a lot we don’t know regarding outcomes of cardiac transplantation in this group. It’s really a new frontier,” Clark added.
“The simple congenital heart disease, as defined by the American College of Cardiology, would probably have different outcomes than if we looked at complex congenital heart disease – those with a systemic right ventricle or those with only one ventricle,” Clark added.