Following strong statements on firearms in 1992 endorsing office-based counseling on gun safety at home and legislation to ban the manufacture, sale and distribution of firearms, the American Academy of Pediatricians (AAP) instituted a periodic survey of its membership to assess follow-up trends.
A new report prepared for the Pediatric Academic Societies 2020 meeting compares responses from a 2019 survey with responses from 1994, 2000, 2007 and 2013. The survey addresses attitudes toward violence as a priority, clinical experience treating gun injuries, personal counseling practices and attitudes toward legislative options.
“The Academy is focused on addressing and improving children’s health; that includes prevention and treatment,” said Shari Barkin, M.D., director of the Division of General Pediatrics at Vanderbilt University Medical Center and an author of the report. “Reducing the number of firearm injuries is an enduring issue. How do we counsel effectively and use evidence to improve child health outcomes?”
“We periodically survey membership on several topics related to counseling. What’s different about this one is that it provides trend data over a long period of time,” said Lynn Olson, Ph.D., vice president of research for AAP and lead author of the study.
Violence Prevention as a Priority
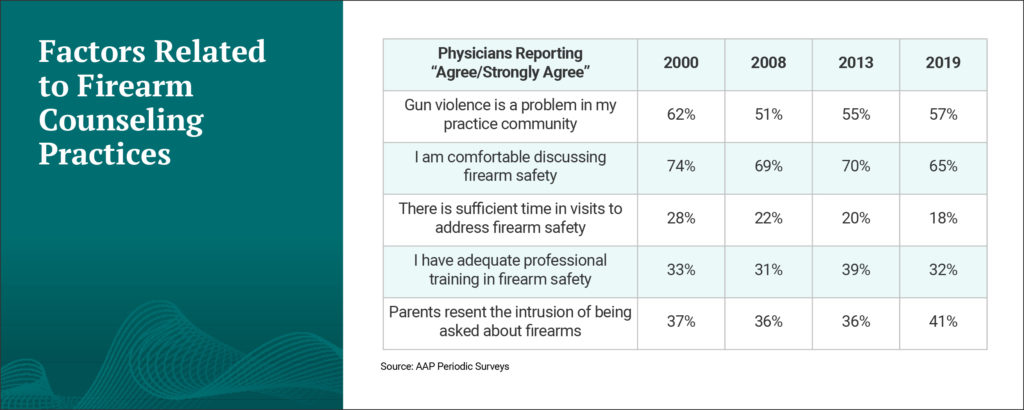
After a decline in violent deaths in children and adolescents between 1999 and 2013, the years since have seen a reversal in this trend. The 2019 AAP survey respondents agree; 57 percent reported that “gun violence is a problem in my practice community.” Across all survey years, 90 percent or more said that violence prevention should be a pediatric priority.
“When you’re looking at the epidemiology of this, 14 percent of pediatricians say that they have treated or consulted on one or more gun injuries in the past 12 months,” Barkin said.
Barkin and colleagues have previously shown that pediatricians can facilitate a reduction in behaviors associated with child violence. In 2008, they published the results of a 5-year, NIH-sponsored trial in Pediatrics that demonstrated the effectiveness of a brief, office-based violence-prevention approach in increasing safe firearm storage. “We showed that information becomes activation with the right tools,” Barkin said.
“14 percent of pediatricians say that they have treated or consulted on one or more gun injuries in the past 12 months.”
Counseling to Prevent Gun Accidents
A majority of physicians surveyed, 65 percent, report they are comfortable discussing firearm safety in the office visit. While this rate has not increased over time, the number of physicians reporting they always or sometimes identify if there are firearms in the home has increased (69 to 77 percent between 2000 and 2019).
In 2019, only 18 percent of respondents agreed or strongly agreed that there is enough time in patient visits to counsel regarding firearm safety and just 32 percent agreed they have adequate professional training. Up from 36 percent in 2013, 41 percent perceive parent resentment as a barrier to counseling.
The way the physician approaches the topic is key, Barkin explained. “Our role should be to discuss firearm safety. An effective, respectful conversation should include all the ways parents can make their homes the safest for children to play and live.”
Advocacy and Training
In 2013, questions regarding legislation were added to the survey. Since the addition, over 84 percent of respondents believe legislation/regulation will help reduce injury or death, and more than 90 percent support legislation to hold gun owners responsible if children are injured or injure others with their guns.
While support for handgun bans has declined, support to ban assault weapons and universal background checks (also added in 2013) is high, Barkin said.
Barkin has received funding from the AAP to turn the data from her research into a multimedia training platform for medical students, residents and pediatricians. “Education is the primary goal,” she said. “We hope to create a community of empowered pediatricians who are comfortable with counseling and can advocate for children’s health.”