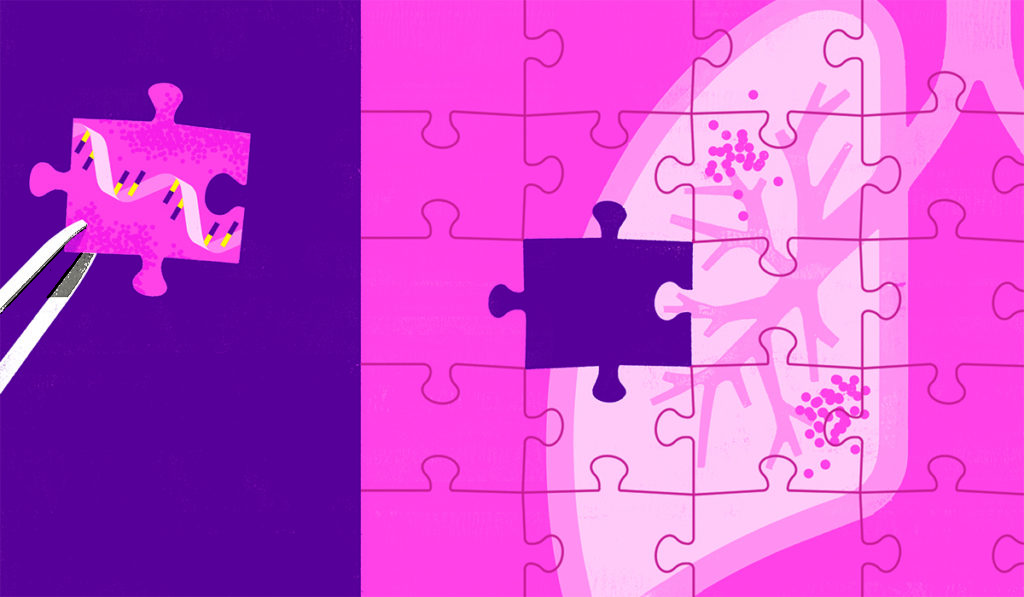
A new single-cell RNA sequencing study helps characterize the cellular landscape of the pulmonary fibrosis lung. The report reveals a dramatic shift in epithelial cell phenotypes in diseased lungs and identifies a novel pathologic epithelial cell type highly enriched in the fibrotic distal lung.
“The mechanisms linking epithelial injury-repair to the dramatic fibrotic remodeling we’ve seen in the lungs of patients with pulmonary fibrosis have been elusive,” said Jonathan Kropski, M.D., a senior author on the study and assistant professor in the Department of Allergy, Pulmonary and Critical Care at Vanderbilt University Medical Center.
“We now have a series of clues as to how epithelial repair mechanisms may contribute to progressive lung fibrosis both directly and through paracrine signaling mechanisms to adjacent mesenchymal cells. This new knowledge may help us address the huge unmet need for better therapies that have more benefit for patients and come with fewer side effects.”
“This new knowledge may help us address the huge unmet need for better therapies that have more benefit for patients and come with fewer side effects.”
The study, published this week in Science Advances, was a collaboration between investigators at Vanderbilt and the Translational Genomics Research Institute (TGen) that included Nicholas Banovich, Ph.D., an assistant professor in TGen’s Integrated Cancer Genomics Division.
A Novel Epithelial Cell Type
The researchers performed single-cell RNA sequencing of cell suspensions of peripheral lung tissue from 20 pulmonary fibrosis lungs and 10 non-fibrotic control lungs.
The sequencing identified a novel epithelial cell state, found almost exclusively in fibrotic lungs, that can produce components of the pathologic extracellular matrix like collagen and fibronectin. The cells can also express high levels of growth factors and cytokines that activate fibroblasts. Further analyses suggested this profibrotic epithelial cell state represented pathologic diversion from a key differentiation program involved in the generation of type 1 alveolar epithelial cells.
“You find these cells localized immediately overlying the regions of the most active collagen and matrix production in tissue,” Kropski explained. “We think they are really crucial in both directly mediating profibrotic remodeling and also in activating local adjacent fibroblast populations to produce the exuberant scarring.”
Cellular Complexity of Lung Epithelium
In addition to shedding light on disease mediators, the high-resolution transcriptomic data revealed that, in general, there is a higher degree of cellular complexity within the lung epithelium than had been appreciated previously.
Classic models of the lung epithelium portray four major cell types within the conducting airways: basal cells, secretory cells, ciliated cells and goblet cells. However, Kropski and colleagues report that there are subsets of secretory cells that express genes canonically associated with other cell types.
“These data suggest that there are a number of discrete types of secretory cells that have distinct gene expression programs, specific localization along the proximal-distal axis of the lung, and potentially, distinct functions in lung repair,” Kropski said.
“There are a number of discrete types of secretory cells that have distinct gene expression programs, specific localization along the proximal-distal axis of the lung, and potentially, distinct functions in lung repair.”
A Springboard for Future Research
Results from the study are serving as a springboard for further research. For example, Nikki Winters, M.D., a pulmonary critical care fellow at Vanderbilt, is using animal models and culture systems to investigate the activation and regulation of uncharacterized fibroblast subtypes identified by the study.
Published alongside the new study is a companion paper by an independent group reporting highly concordant findings using a slightly different single-cell platform.
“One of the things that we’ve been very excited about is that these single-cell sequencing platforms appear to facilitate reproducible data across different centers and across different basic tissue processing, which gives us confidence in the strength and the robustness of the findings,” Kropski said.