Long considered compensatory and helpful, left ventricular hypertrophy (LVH) in response to pressure overload from aortic stenosis (AS) actually has adverse consequences, according to two recent studies. The research suggests that earlier aortic valve replacement before LVH becomes severe, may be warranted even in the absence of symptoms.
“Increased hypertrophy before transcatheter aortic valve replacement (TAVR) is associated with worse clinical outcomes,” said Brian R. Lindman, M.D., medical director of the Structural Heart and Valve Center at Vanderbilt University Medical Center. The first study appeared in the Journal of the American College of Cardiology: Cardiovascular Interventions. Holly Gonzales, M.D., an assistant professor of medicine at Vanderbilt, was the first author.
“Increased hypertrophy before transcatheter aortic valve replacement (TAVR) is associated with worse clinical outcomes.”
The second study, published in The Journal of the American College of Cardiology, looked at the association between left ventricle mass index (LVMi) regression, a measure of the extent to which the hypertrophy had receded, at one year after TAVR and clinical outcomes up to five years post-TAVR.
“For patients who had moderate or severe LVH before TAVR, the extent to which the ventricle remodels after the procedure matters a lot in terms of how those patients will ultimately do with respect to rehospitalization and long-term survival,” Lindman said.
Critical Question of Timing
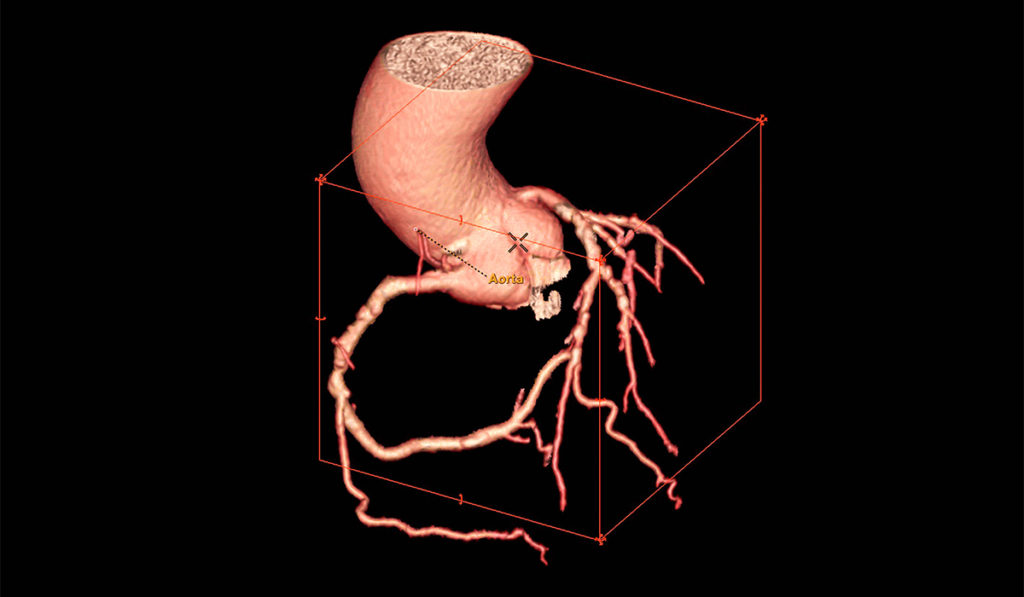
In AS, the aortic valve fails to open fully because its leaflets have thickened and calcified, reducing the left ventricle’s pumping ability and raising the pressure within it. Lindman explained that in many cases, the heart wall thickens and LVH develops, which reduces stress on the ventricle’s walls.
The only treatment that improves the quality of life and extends survival for patients with AS is aortic valve replacement, after which the LVH recedes to a greater or lesser extent. “There are no medications that slow progression of AS or improve clinical outcomes for these patients,” Lindman said.
A key question has been the timing of either open surgery or TAVR. Until now, Lindman says valve replacement has only been recommended in the presence of severe, symptomatic AS. In the absence of symptoms, certain triggers have been viewed as reasonable prompts for valve replacement but significant LVH has not numbered among them.
Risks of LVH
The first study followed 4,280 patients across several trials who had severe symptomatic AS and underwent TAVR. The 1,550 patients with severe LVH, compared to those without LVH, experienced an adjusted 16 percent increase in the risk of all-cause death, 26 percent increase in the risk of cardiovascular death, and a 45 percent increase in the risk of rehospitalization out to five years.
“The study suggests that severe LVH ought to be included alongside other potential triggers for valve replacement in the absence of symptoms,” Lindman said.
He notes prior studies of the association between LVH severity and clinical outcomes after valve replacement for AS have yielded mixed results, and have been hampered by the small size and limited follow-up.
“The study suggests that severe LVH ought to be included alongside other potential triggers for valve replacement in the absence of symptoms.”
Benefits of LVH Regression
The second study tracked outcomes among 1,434 patients with moderate or severe LVH who were at intermediate to high risk for surgery and underwent TAVR. Greater LVMi regression at one year was associated with a lower risk of death, and rehospitalization between one and five years.
The regression of LVH after TAVR was not universal. Compared to those with no LVH at one year, residual severe LVH was present in 39 percent of patients at one year and was associated with a 71 percent increase in the risk of death and an 89 percent increase in the risk of rehospitalization between one and five years.
Mounting Evidence Against Dogma
”Together, our two studies challenge the long-standing assumption that cardiac hypertrophy in response to AS is compensatory, necessary and helpful,” Lindman said.
“Our two studies challenge the long-standing assumption that cardiac hypertrophy in response to AS is compensatory, necessary and helpful.”
“First, the findings suggest that in patients with severe AS and severe LVH, prompt valve replacement may be warranted even before symptoms arise,” he added. “Second, the data suggest a potential role for adjunctive medical therapy targeting LVH, either to prevent its development in the face of ongoing pressure overload from AS prior to valve replacement or to augment its regression after valve replacement.”
Both approaches are now being tested in several ongoing clinical trials, Lindman said.