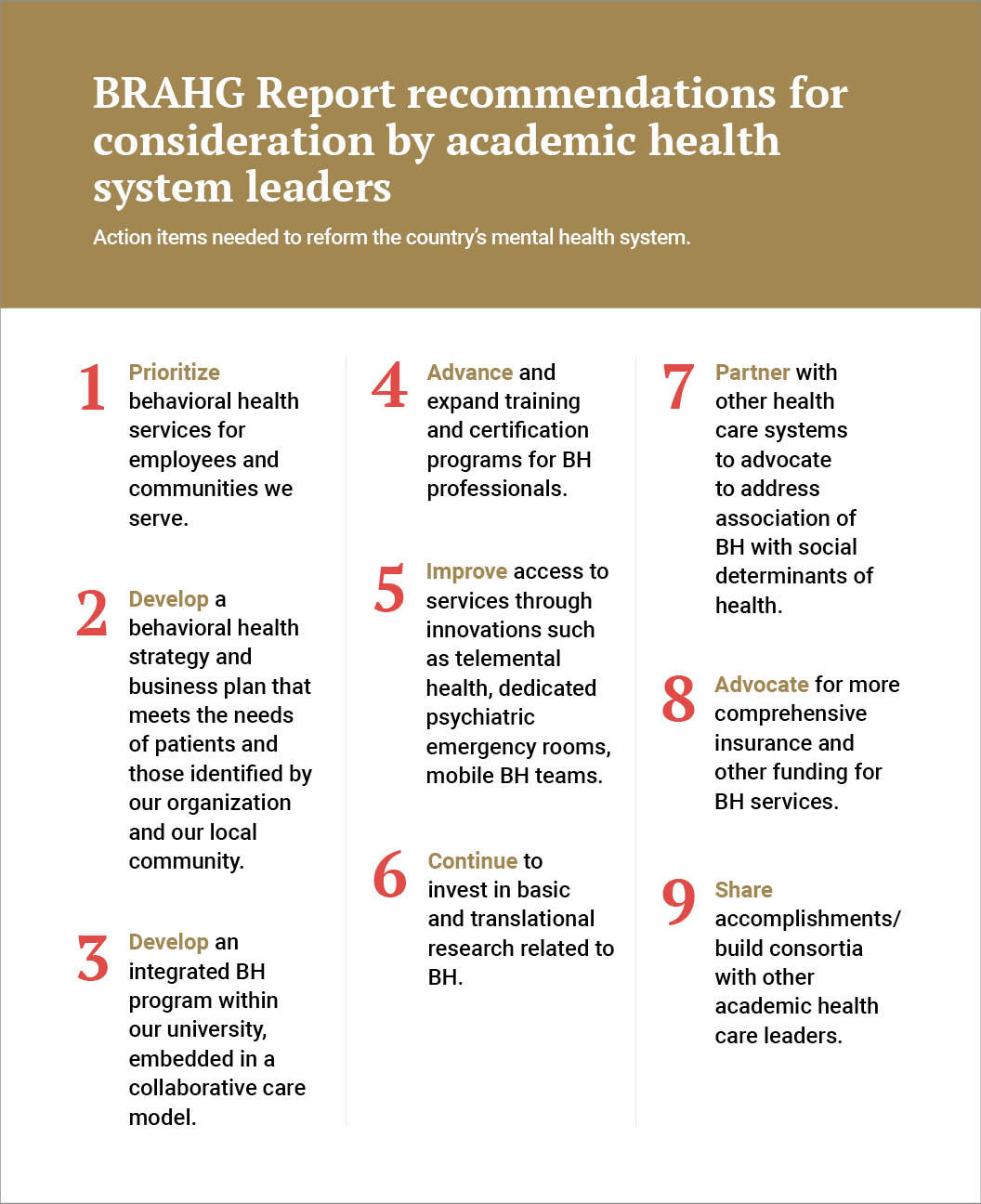
Leaders from a group of academic medical centers have come together to identify shortfalls of the current mental health system and identify areas of change within their sphere of influence. The Blue Ridge Academic Health Group (BRAHG) report emerged from a June 2019 meeting of the group co-chaired by Jeff Balser, M.D., president and CEO of Vanderbilt University Medical Center. The report establishes nine action items for reform, ranging from workforce development to advocacy (see chart below).
“There are probably three of these action areas that we, as academic medical centers, can substantially impact,” said Stephan Heckers, M.D., chair of the Department of Psychiatry and Behavioral Sciences at Vanderbilt. Heckers is leading the charge to implement the recommendations at Vanderbilt.
“We can train more behavioral health professionals, work toward embedding more services into collaborative care, and more aggressively pursue basic and translational research to help guide treatment. The rest will require political will for funding, followed by a building process,” Heckers said.
“There are probably three of these action areas that we, as academic medical centers, can substantially impact.”
A Complex and Broken System
The report recounts how, historically, repairs on a badly flawed system were aborted. The Community Mental Health Act of 1963 legislated a dismantling of the notorious asylum system, to be replaced by a network of smaller, community-based mental health centers. Though the Act allocated funds to build 2,000 centers, the legislation didn’t provide money needed to operate the centers long term.
Over 50 years later, there remains an inadequate patchwork of underfunded community health centers. More severely mentally ill people are in prison than in institutional care. About 90 percent of beds have been cut at the remaining state hospitals, and the BRAHG report notes available inpatient psychiatric beds have dropped from 339 per 100,000 people to 11. With these shortages and early intervention services scarce, people with mental illness are flooding EDs.
Focus on Reimbursement
The report states that one in five adults experience mental illness each year, while diagnoses among college students are on the rise and resources for at-risk children are inadequate. Not enough headway has been made in the battle against substance abuse. The data also point to concerning trends in dysfunctional lifestyle habits and a general “epidemic of loneliness.”
Heckers considers the current behavioral health (BH) reimbursement system a particularly insidious disincentive to expanding services. Average reimbursement rates for primary care office visits are 23.8 percent higher than behavioral reimbursements, even when treating the same condition, like depression. As a result, about half of psychiatrists do not accept any public or private insurance.
To help, the BRAHG report suggests academic health centers “can and should” explore value-based care and “provide leadership in transitioning from entrenched fee-for-service reimbursement payer arrangements.”
Changing the BH Care Model
Heckers says a key focus area for Vanderbilt will be the growing shortage of psychiatrists. While there has been an uptick in interest and residency slots in psychiatry, the replacement rate lags the high retirement rate across the profession. “Academic centers are not going to be able to make a huge dent in filling the gap – we simply cannot train people fast enough,” Heckers said.
To bolster its ability to provide services through psychiatrists and other medical providers, Vanderbilt is adding additional training slots – residencies, fellowships and specialized programs – that focus on addiction psychiatry, geriatric psychiatry, and child and adolescent psychiatry.
Additionally, Vanderbilt is working to foster interprofessional, side-by-side learning between residents, fellows and nurse practitioners within and outside the realm of psychiatry. The hope is that more interprofessional training will flow into more embedded psychiatric services.
“The vast majority of BH issues can be dealt with outside of medical systems, or if they are in medical systems, with psychiatric nurse practitioners, master’s-degreed counselors or social workers,” Heckers said. “Integration of psychiatric services into medical services not only addresses patients’ depression and other BH issues, but we know that their overall health gets better and the utilization of health services is lower.”





