Noncyclic chronic pelvic pain (CPP) – unrelated to dysmenorrhea, dyspareunia, dyschezia or dysuria – is common but often challenging to diagnose. Its causes are poorly understood, and determining pain is complicated, because it is rarely associated with one condition.
Because of CPP’s complexity, it is also difficult to define. One review defined noncyclic CPP as “pain that has persisted for more than three months, is localized to the anatomic pelvis (lower abdomen below the umbilicus), and is of sufficient severity that it causes the patient to become functionally disabled or to seek medical care.”
Musculoskeletal, neurological, gynecological, gastrointestinal and urological disorders may all cause CPP. A patient may have endometriosis, interstitial cystitis, pelvic inflammatory disease, IBS, myofascial disorders, neuropathy or a spastic pelvic floor, which can affect several systems.
“The hardest part of my job is convincing women that the pain is not just in their uterus.”
“The pelvis is the home for many organ systems and the systems can feed off each other,” said Amanda Yunker, D.O., of Vanderbilt University Medical Center’s Division of Gynecologic Minimally Invasive Surgery. “It’s like an orchestra, once one system starts playing they all chime in. Just because someone is diagnosed with endometriosis, it doesn’t mean they can’t have something else. The hardest part of my job is convincing women that the pain is not just in their uterus.”
Identifying CPP’s Source
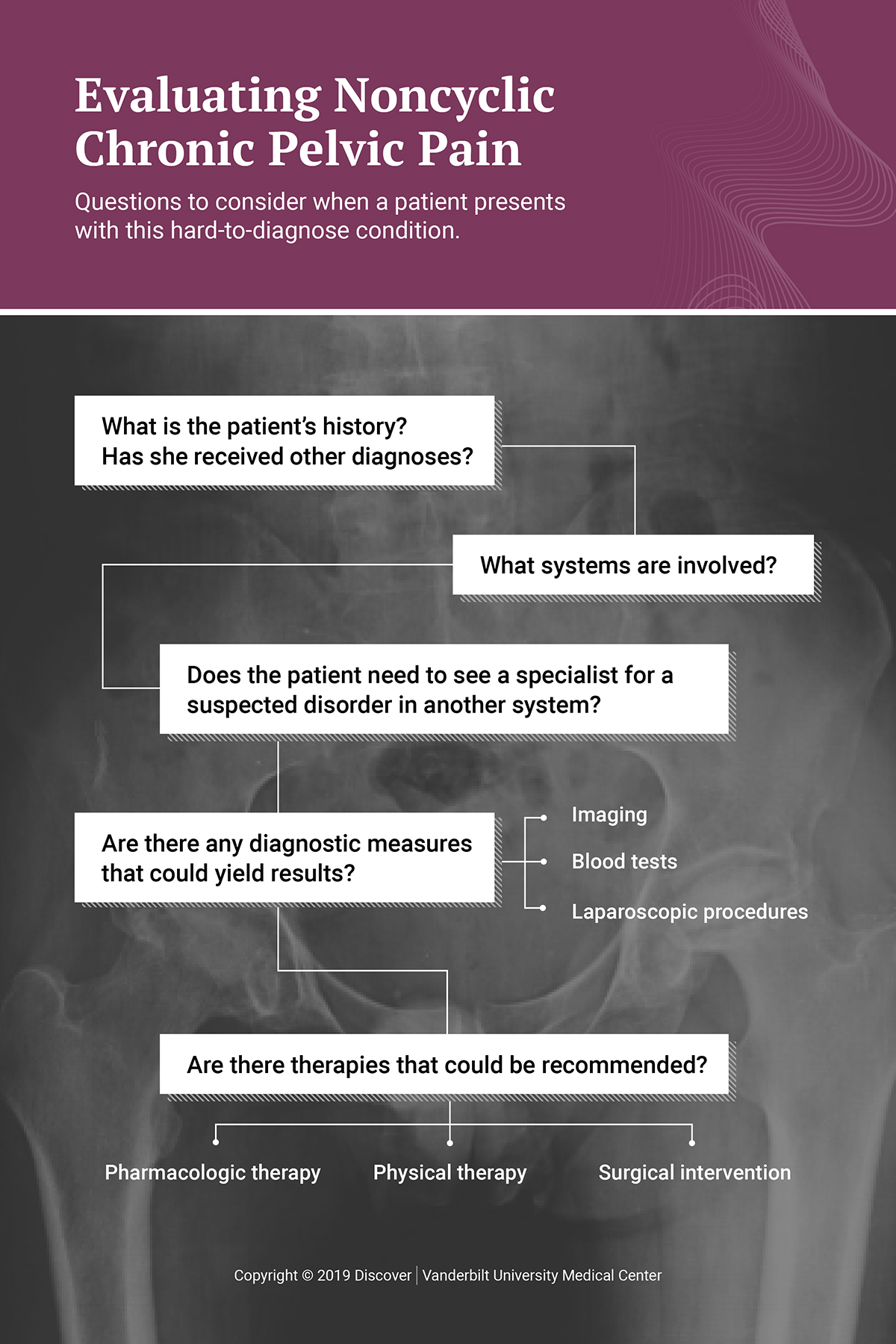
Determining CPP etiology is best accomplished through experience and observation in a clinic that sees many cases. Yunker and her gynecology colleagues at Vanderbilt Women’s Health get referrals from PCPs, OB/GYNs and other specialists. They also see patients who may have been diagnosed and treated for pain that hasn’t gone away.
“We provide pelvic pain problem-solving,” Yunker said. “We don’t just think like GYNs, we look at every system, including the brain and how the patient processes pain and other stimuli. Ninety percent of what we learn comes from history and from listening to the patient. We’re methodical in teasing out what might be wrong.”
“We look at every system, including the brain and how the patient processes pain and other stimuli.”
The goal is to identify the initial source of the CPP—how it started, location and patterns. Yunker sometimes aids her diagnosis by incorporating an ultrasound or other pelvic imaging to ensure the anatomy is normal, or to rule out cysts, tumors or possible iatrogenic issues. “But there’s a limitation to what imaging can pick up.”
Blood tests can help diagnose some conditions. However, if the pain’s cause cannot be determined through basic testing, diagnostic laparoscopy is often recommended. “Someone who is highly skilled in laparoscopic surgery can look at all the organs and diagnose, and often treat, the problem,” Yunker explained. “If we suspect a disorder in another system, we refer the patient to the appropriate specialist for further testing and/or pain management.”
Treating CPP
A wide range of therapeutic interventions may be used to treat CPP, dependent on the etiology. Pharmacologic therapies include analgesics, antidepressants, hormonal therapies, antineuropathic agents and neuromuscular blocking agents. Surgical intervention is used either to remove the pathology causing the CPP or to interrupt the nerves that transmit the pain impulses. Surgery may include excision of endometriosis, lysis of adhesions or hysterectomy. Other non-surgical approaches include counseling, pelvic floor physical therapy and complementary therapies.
CPP can significantly impact quality of life, causing depression, fatigue, sexual dysfunction and physical limitations. Many patients lose work due to disabilities associated with the pain. Taking a more comprehensive approach can help physicians identify causes of the pain early and get the patient in treatment before CPP becomes a burden.
“The key is collaboration,” Yunker said. “We have to listen to our patients and partner with them. The goal is to provide strategies that will help them stay healthy and improve their quality of life.”