A gamma knife or a linear accelerator (LINAC) are commonly used to ablate severe essential tremor and to treat tremor-dominant Parkinson’s disease. While their success rates hover around 80 percent, researchers at Vanderbilt University Medical Center are working to shrink the margin of error and better identify tremor sites of origin.
Radiation oncologist Austin Kirschner, M.D., medical physicist Guozhen Luo, M.S. and Vanderbilt colleagues published a study in 2017 that demonstrated the benefits of a LINAC over a gamma knife as offering an equally precise, but non-invasive, alternative with a shorter procedural time.
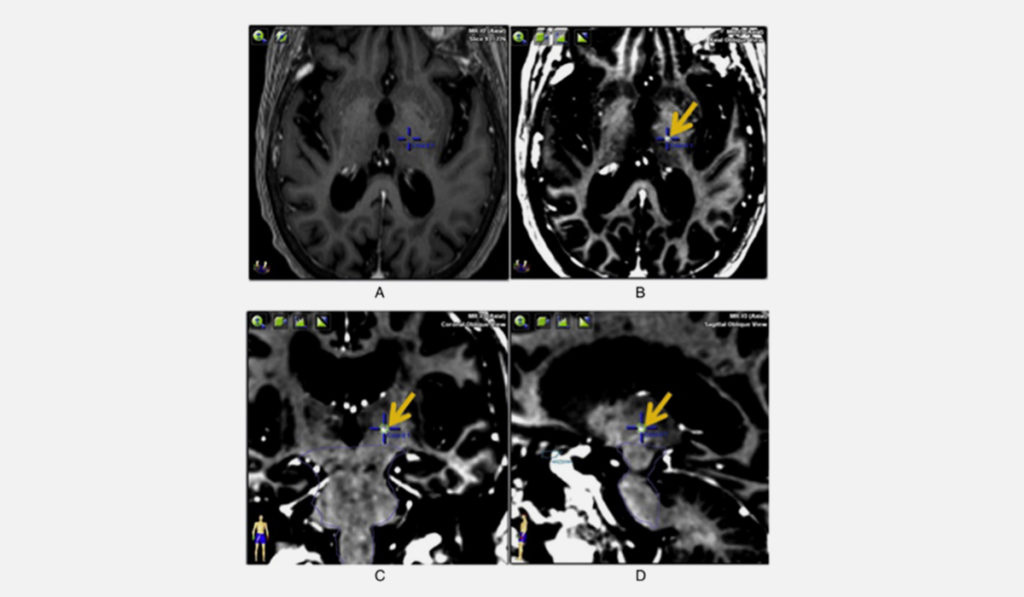
They will soon publish encouraging patient outcomes from using a new neuroanatomical brain atlas, guided by Brainlab ExacTrac® software, to more accurately target tremors. “Instead of the standard method of using a historical atlas from surgical series, here we are looking at customized anatomical targets, based on the shapes and sizes of human neuroanatomy and the patient’s own MRI, to home in more precisely on the origins of their tremor,” Kirschner said.
“We are looking at customized anatomical targets, based on the shapes and sizes of human neuroanatomy and the patient’s own MRI, to home in more precisely on the origins of their tremor.”
The Ablation Alternative to Surgery
Patients generally receive ablative treatment because medication has failed and they don’t want or are not candidates for surgical implant with a deep brain stimulator, Kirschner said. The stereotactic ablation is a relatively low-risk alternative, though treatment errors are not necessarily benign. “This is a regulatory center for the brain. If you are off the target, it could be that the treatment is ineffective or another movement disorder or weakness could result,” Kirschner said. “These can be transient or permanent.”
Kirschner explained that in LINAC ablations, radiation enters the brain through 20 arcs that form a spherical pattern, each arc carrying a very low dose. They intersect in the ventral intermediate nucleus of the thalamus, the site of the tremor, delivering a high dose of 160 gy. This high dose enables ablation in a single fracture.
“With a brain tumor or glioblastoma, we may use 60 gy over 30 treatments. Here, we use a tiny aperture only 4 mm wide. With such a fine-tuned dose, we get minimal scatter, minimal radiation exposure anywhere else in the brain. It’s really well-tolerated,” Kirschner said.
LINAC or Gamma Knife
For decades, framed stereotactic radiosurgery with a gamma knife has been the gold standard for tremor ablation. While it can target the tremor site within a millimeter error margin, there are drawbacks. A hard frame is used, with screws inserted down to the skull, and the procedure can extend for several hours, lengthening over the five-year half-life of the machine’s cobalt supply.
Using LINAC with ExacTrac® software, Kirschner and his colleagues have been able to match the gamma knife’s accuracy and supply predictable treatment times, while using a non-invasive, “frameless” mask that holds the patient’s head in place without piercing the skin.
An Atlas for Refractory Patients
Kirschner’s team is also testing alternative approaches to close in on the minority of patients who are not yet helped by the procedure. A new neuroanatomical “atlas” could offer significantly greater precision in identifying the tremor site origin.
The atlas allows radiosurgeons to target using a preexisting library of brain images and the individual MRI of each patient’s brain. Kirschner said, “There is a ‘map’ of how that anatomy is supposed to look, and the software figures out how to match that to the patient’s brain MRI.”
Kirschner is also exploring a functional targeting technique to ablate tremors. This involves using diffusion tensor imaging, a kind of MRI sequence, to target the tracts the neurons take – the lengths of the axons in the brain. “It may be that disrupting the tract is a better way to target the tremor,” Kirschner said.