Excessive prescribing of opioids after surgery has been recognized as a significant contributor to the opioid epidemic. “On average six to eight percent of patients who are opioid naïve prior to surgery are new, persistent opioid users at three to six months after surgery,” said Jennifer Robles, M.D., assistant professor of urology at Vanderbilt University Medical Center.
Robles and colleagues, including Matthew Resnick, M.D., assistant professor of urologic surgery and health policy at Vanderbilt, have studied prescribing trends in urologic surgery and found that postoperative opioid prescribing varies widely among urologists – ranging from zero to 7,560 mg oral morphine equivalents. The research was presented at last year’s American Urological Association Annual Meeting in Chicago.
“There are no specialty specific guidelines about what we should be prescribing people after surgery,” Robles said. “There are recommendations for some specialties – for general surgery, the Michigan Opioid Prescribing Engagement Network has prescribing recommendations. But by and large, there’s really no literature out there to tell people what they should be prescribing after different procedures.”
Postoperative Opioid Prescribing
Using national Veteran’s Administration data from 2014 to 2016, Robles and colleagues analyzed postoperative opioid prescribing for eight major urologic surgical procedures. The median amount prescribed was found to be 225 mg oral morphine equivalents, which is already greater than one published recommendation of 200 oral morphine equivalents or less following major surgery. In addition, 25 percent of patients received more than 300 mg oral morphine equivalents, and five percent received more than 600 mg oral morphine equivalents – more than three times published recommendations.
“There was an incredible amount of variation, even more than what we expected,” said Robles.
The researchers also compared prescribing trends following open versus minimally invasive approaches for three procedures: radical prostatectomy, radical nephrectomy and partial nephrectomy. They found almost no difference. “This indicates that what providers are prescribing is roughly the same, regardless of whether the patient had an open or less invasive procedure,” Robles added.
“What providers are prescribing is roughly the same, regardless of whether the patient had an open or less invasive procedure.”
“One of the big promises of minimally invasive surgery is that it causes less pain, and that patients would need less pain medicine,” Robles said. “As inpatients, these patients may have been given different pain regimens, but what they are sent home with is the same.”
Regional Differences
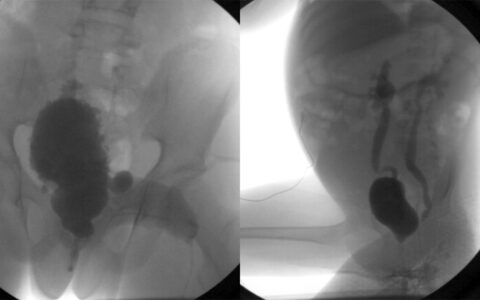
The Centers for Disease Control and Prevention (CDC) reports that overall opioid prescribing varies strongly by region, and Robles found there to be similar regional differences in opioid prescribing among urologists.“If you look at the CDC map in 2015,” she said, “California has one of the lowest rates of overall opioid prescribing and Oregon has one of the highest rates. We see a similar trend in our dataset.” In Oregon, 71 percent of opioid prescriptions following major urologic surgery were in the highest quartile, while in California only 16 percent of prescriptions were in the highest quartile.
In contrast, Robles reports that preoperative opioid use explained less than one percent of the observed variance in prescribing among urologists.
Bringing About Change
The regional prescribing trends suggest to Robles that modifiable cultural factors play a major role in driving prescribing patterns. “I think a big part of this entire surgical over-prescribing problem is just lack of knowledge – people not knowing how much to prescribe and not realizing that what they prescribe may be very different from what their neighbor prescribes for the same procedure.”
“A big part of this entire surgical over-prescribing problem is just lack of knowledge.”
Several states have recently passed laws restricting initial opioid prescribing; Tennessee’s 2018 law capping initial prescribing at 180 oral morphine equivalents is one of the strictest. Robles says laws like these are bringing about change overnight. Templated order sets or decision support tools integrated into prescribing software are other avenues that may help communicate procedure-specific prescribing recommendations.