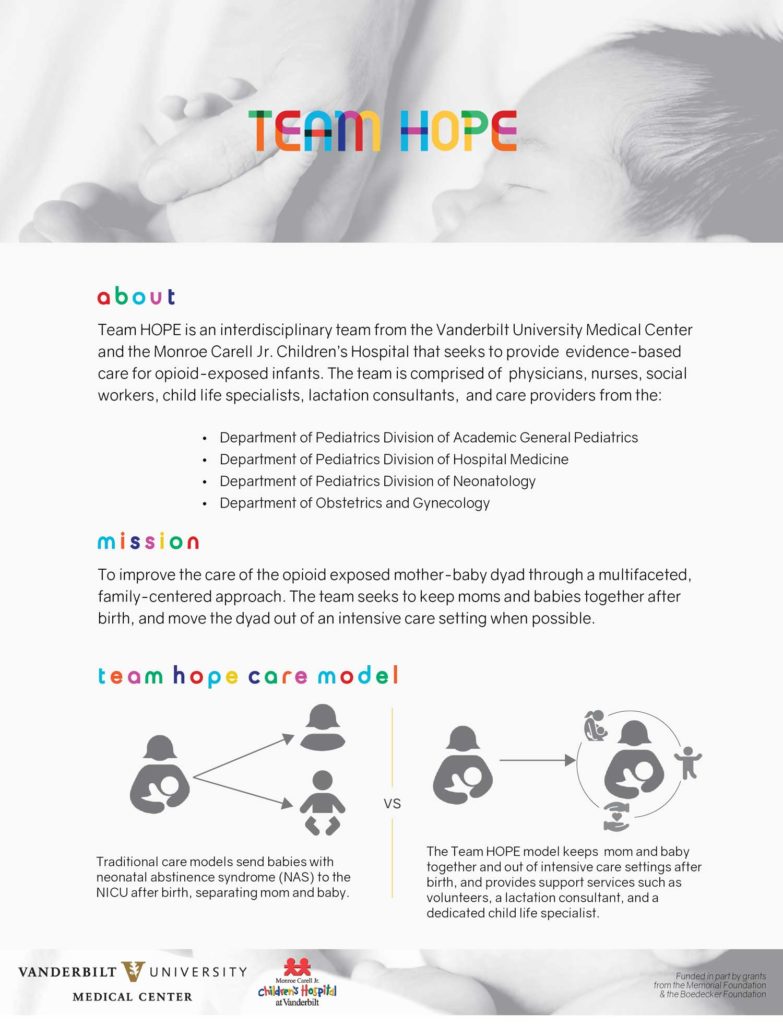
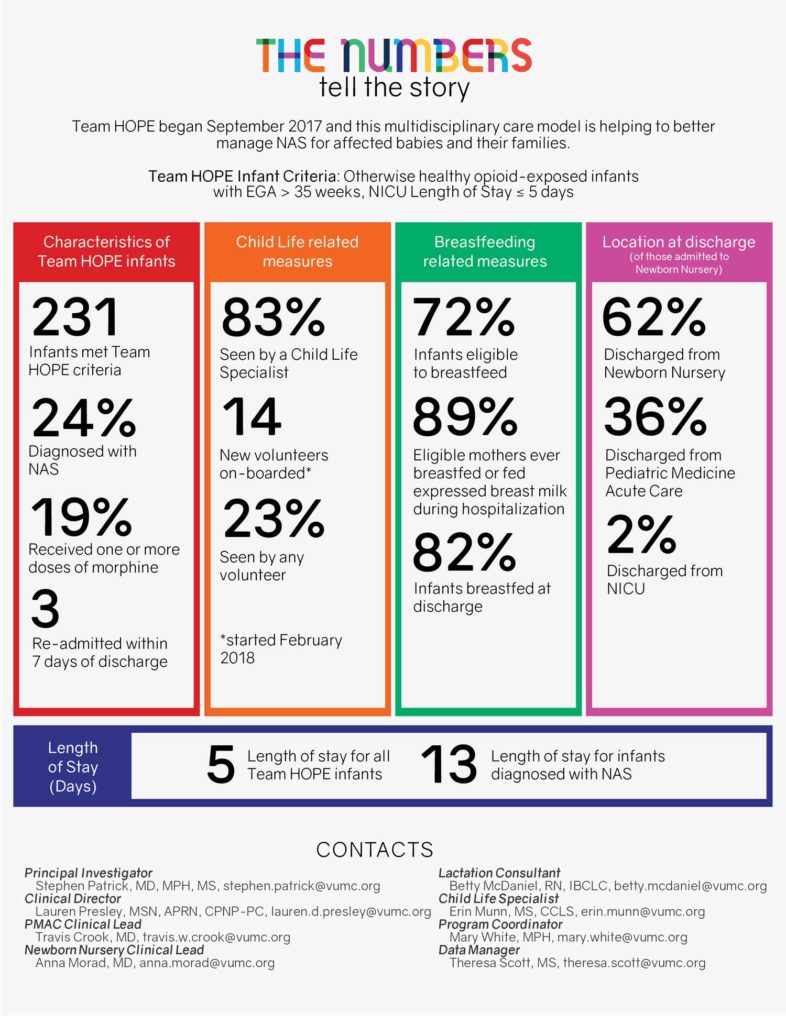
A collaborative program at Vanderbilt University Medical Center and Monroe Carell Jr. Children’s Hospital at Vanderbilt is changing the way nurses and doctors care for newborns diagnosed with neonatal abstinence syndrome (NAS). Started in 2017, the Team Hope program has instituted a variety of evidence-based practices to improve the care of opioid-exposed infants and their mothers, with an emphasis on family-centered interventions.
This year a Team Hope pilot-tested a standardized discharge bundle to streamline referrals of opioid-exposed neonates to appropriate post-discharge services, like the pediatric development clinic. The study was published in a special issue of Hospital Pediatrics focused on NAS.
“Infants exposed to opioids and their families face a variety of obstacles and risks that can impede follow-up care,” said Travis Crook, M.D., assistant professor of pediatrics in the Division of Hospital Medicine and lead author on the study. “The pilot stemmed from our mission to improve the care of infants and families affected by opioid use by extending the opportunity for good health beyond the hospital walls.”
“Infants exposed to opioids and their families face a variety of obstacles and risks that can impede follow-up care”
Pre-discharge Checklist
The bundle implements a discharge checklist designed to ensure infants and their families are connected with comprehensive follow-up services. Before implementation, only 2.6 percent of infants had a fully completed discharge bundle, which includes tailored referrals to a primary care physician, early intervention services, in-home nursing assessment and educational services, a development clinic (if diagnosed with NAS), and gastroenterology/infectious diseases clinics (if the baby was exposed to hepatitis C).
Six months after implementation of the checklist, 60.3 percent of qualified infants had completed the discharge bundle. The focus on completing a checklist at discharge for every affected infant — a low-cost intervention — illustrates how coordination between a care team of physicians, social workers, nurses and patient advocates can bridge community resources.
“Nationally, we know there are gaps in connecting families affected by the opioid crisis to services that could help them thrive,” said Stephen Patrick, M.D., director of the Vanderbilt Center for Child Health Policy and senior author. “A simple checklist, coupled with rigorous quality improvement methodology, helps us do a better job of connecting families to these important community resources.”
“A simple checklist, coupled with rigorous quality improvement methodology, helps us do a better job.”
Model of NAS Care
Infants with NAS are more likely to experience respiratory complications and feeding difficulty, be born with low birth weight, and have longer lengths of stays in the hospital following birth, Patrick said. Team Hope’s mission is to reduce NAS symptoms and complications with multidisciplinary support.
Team Hope includes Vanderbilt specialists from the Newborn Nursery, the Neonatal Intensive Care Unit and Obstetrics at Children’s Hospital along with Child Life, social workers and lactation consultants working together to institute evidence-based practices that improve care consistency for opioid-exposed infants.
“We’ve changed the model of care,” Patrick said. “When these babies have a long stay, they go to a general inpatient floor unless they have other complications, and moms and babies can room together. We promote bonding and breastfeeding with a dedicated lactation consultant and Child Life specialist. We engage the family and coordinate volunteers on how to help the baby improve.”
Hopeful Outcomes
In its two-year existence, Patrick says Team Hope has already reduced length of stay and readmissions, improved child life-related measures, increased breastfeeding, and moved more babies from the NICU to the newborn nursery pre-discharge.
“The root of Team Hope’s mission is to change the paradigm from doctors directing care to helping families get what they need to be successful,” Crook added. “This work is one step forward in our journey to provide better care for our families.”