The Tourette Syndrome Clinic at Vanderbilt University Medical Center has joined fewer than 20 centers nationwide in receiving designation as a Center of Excellence from the Tourette Association of America. David Isaacs, M.D., an assistant professor of neurology, and Heather Riordan, M.D., an assistant professor of child neurology, are leading the multidisciplinary team at the clinic, that now includes a neuropsychologist and two occupational therapists.
“The more we know about Tourette syndrome, the more we see that motor and vocal tics are often just the tip of the iceberg in terms of patients’ challenges,” Isaacs said. “We are assessing and treating not only tics but also the psychiatric and psychological symptoms that are often associated with the syndrome.”
Bringing Care to “No Man’s Land”
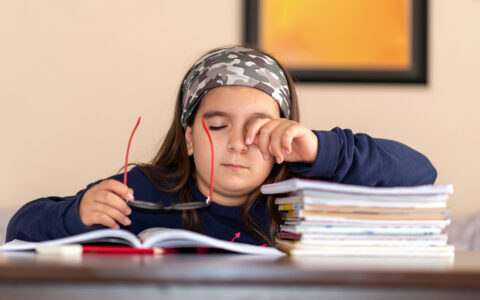
Though Tourette syndrome affects as many as 300,000 children in the U.S. – around one in 160 – Riordan and Isaacs say that many affected children and adults are falling under the health care system’s radar. While most patients’ symptoms attenuate greatly by age 20, in about one-third of cases the symptoms persist into adulthood, Isaacs says.
“Many of the adult patients I see with Tourette syndrome have struggled to find appropriate resources because it is often considered a pediatric syndrome,” Riordan said. “They can find themselves in a kind of ‘no-man’s land,’ with few providers who treat the complex of conditions they often face.”
Beyond Tics
Last year, Isaacs and Riordan published a study showing that for adult patients, psychiatric symptoms – in particular depression – have a greater impact on quality of life than tics.
“The more we know about Tourette syndrome, the more we see that motor and vocal tics are often just the tip of the iceberg in terms of patients’ challenges.”
The Comprehensive Behavioral Intervention for Tics (CBIT) protocol used at the clinic is a program that helps patients learn to anticipate and create a competing response to tics. To address broader concerns, the clinic’s team also teaches relaxation and emotion regulation techniques that help not just with tics but with the anxiety, depression and obsessive-compulsive symptoms associated with the cortico-striato-thalamo-cortical loop dysfunction thought to be at the root of Tourette syndrome.
Isaacs’ hope is that achieving the Center of Excellence designation for Tourette syndrome will attract adult patients who may have given up on treating their condition long ago. “We want to show them that it’s not too late to address both their tics and psychiatric comorbidities and start feeling better.”
Environmental Stressors
The team is launching new studies to explore the prevalence and potential role of environmental stressors in Tourette syndrome.
“In one, we’re assessing mental health and environmental stressors in adolescents with and without Tourette syndrome in order to understand possible relationships between these domains,” Isaacs said.
In an adult counterpart to this study, the researchers are performing detailed, longitudinal phenotyping of adults with Tourette syndrome, incorporating a standardized instrument to assess the lifetime history of major and minor environmental stressors. Their objective is to determine how stressors may affect the long-term clinical trajectory of those with Tourette syndrome.
“We hypothesize that those individuals with greater burden of lifetime environmental stressors will have greater burden of psychiatric symptoms,” Isaacs said. “This work, we believe, will draw attention to the need for comprehensive care for adults with Tourette syndrome, care that must extend beyond tics and begin to systematically incorporate psychosocial health.”
Medication Management
Controlling tics is still at the root of Tourette syndrome care, and Isaacs says ecopipam is a promising new medication currently under study.
“We want to show them that it’s not too late to address both their tics and psychiatric comorbidities and start feeling better.”
Emalex Biosciences, the maker of ecopipam, recently completed a multinational phase 2b pediatric trial of this dopamine receptor antagonist, with Isaacs as primary investigator for the Vanderbilt site.
“Early phase studies have shown ecopipam is well-tolerated and reduces tics,” Isaacs said. “The evidence to date suggests it may effectively work without the side effects of weight gain, sedation or involuntary movements that can accompany currently available treatments.”
Education and Collaboration
Riordan says the staff at the Tourette Syndrome Clinic are also working beyond the clinic walls. “A lot of what we do is aimed at raising awareness in the medical community, as well as in the general public,” she said.
The clinic hosts a Tourette syndrome working group, composed of neurologists, psychiatrists, psychologists, pharmacists, nurses, basic scientists and students who assemble monthly to share perspectives, case studies and research.
“We really focus on community engagement, educating each other about what is known about Tourette syndrome, but also about the gaps in care and research,” Isaacs said. “Our working group has become a wonderful network that helps all of us participating to learn from each other, with the goal of providing the best, most up-to-date care possible.”