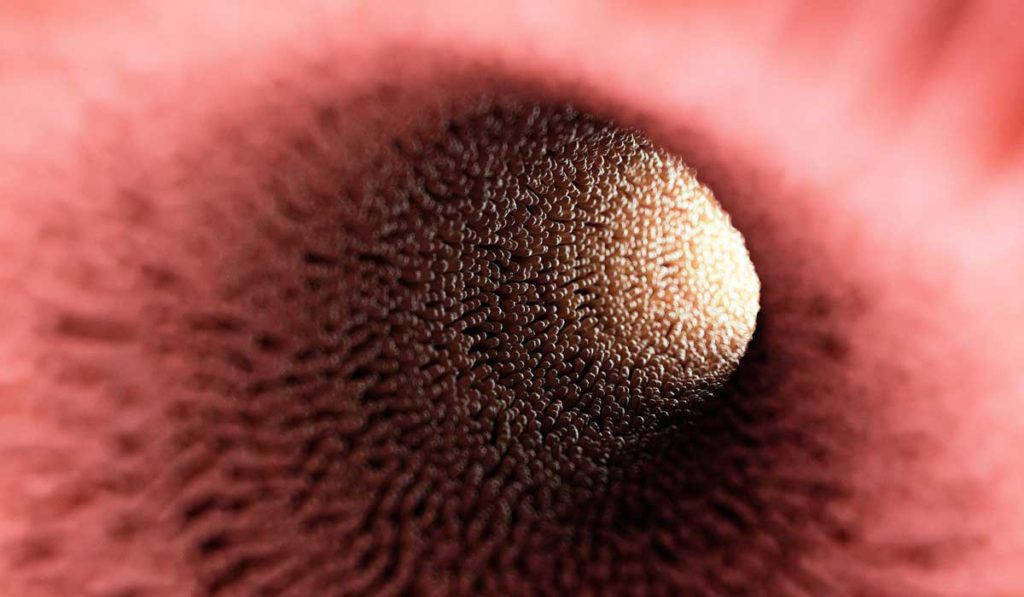
Intraepithelial lymphocytes (IELs) dwell in between the cells of the intestinal epithelium and are considered the sentinels of the immune system due to their critical location at the interface between the core of the body and the outside environment.
“They are the first line of defense against antigenic stimulus in the lumen. They protect against invading pathogens,” said Danyvid Olivares-Villagómez, Ph.D., assistant professor in the Department of Pathology, Microbiology and Immunology at Vanderbilt University Medical Center.
If left unchecked, however, IELs can promote aberrant inflammation and the development of inflammatory disease. A study recently published in PLoS ONE, of which Olivares-Villagómez is senior author, reports that a subpopulation of IELs regulates the survival of another group of IELs, shedding mechanistic insight into IEL homeostasis critical for the regulation of intestinal inflammation.
IELs
While the majority of IELs are antigen-experienced T cells, a subset of IELs do not display T cell receptors (TCRs) and are termed TCR negative IELs.
“Most IEL studies focus on TCR positive cells,” Olivares-Villagómez said. “A few years ago, however, we started realizing that there are also lymphoid cells that are TCR negative and that these cells play important roles for immune responses. At the time, we had never looked to see whether there are IELs that are TCR negative.”
Upon analyzing the IEL compartment for TCR negative cells, Olivares-Villagómez discovered a new population of cells, termed iCD8 alpha cells, that are both TCR negative and express high levels of the transmembrane glycoprotein CD8 alpha. iCD8 alpha cells are important during early immune responses, having the ability to process antigens and engulf and kill bacteria.
Cross-talk between IELs
The new study reports that iCD8 alpha cells can also function to promote the survival of another group of IELs, termed ILC1-like cells. These cells resemble innate lymphoid cells (ILCs), and their dysregulation can lead to disease. ILC1-like cells have been shown to contribute to the development of colitis in mouse models and they are found at high levels in patients with Crohn’s disease.
Olivares-Villagómez made the initial observation that the two cell populations may communicate while characterizing a new animal model. “Depletion of CD8 alpha in these animals not only caused iCD8 alpha cells to disappear, but levels of ILC1-like cells were reduced. This was really strange because ILC-1 like cells do not express CD8 alpha.”
The link was the secreted phosphoprotein osteopontin. iCD8 alpha cells were shown to be a key source of osteopontin within the IEL compartment and osteopontin was shown to promote the survival of ILC1-like IELs. Depletion of iCD8 alpha cells in an animal model of intestinal inflammation caused a reduction in inflammation, while administration of osteopontin increased disease severity.
Finding the Balance
Osteopontin is an intriguing molecule, Olivares-Villagómez said. “It seems to do a lot of things and it is expressed by many different cell types.” Originally discovered in bone, osteopontin is involved in physiological processes, like biomineralization, as well as pathological processes, like cancer and inflammation.
Due to its critical role in multiple diseases, osteopontin is being explored as a therapeutic target. However, Olivares-Villagómez has concerns about this approach.
“We’ve shown that osteopontin is a relevant protein which you may not want to target. When is osteopontin necessary and when is it detrimental? It’s a balance we need to figure out.”
Olivares-Villagómez’s ongoing research is aimed at determining if other cells in the intestinal epithelium regulate IEL survival and whether osteopontin plays a role.