Earlier this month, 20-year-old Disney star Cameron Boyce died suddenly from what was most likely sudden unexpected death in epilepsy, or SUDEP. In this rare complication from epilepsy, a patient who is otherwise healthy dies during or following a seizure, and postmortem examination reveals no structural or toxicological cause for death. Boyce’s family confirmed he had epilepsy.
SUDEP occurs in about 1-2 per 1,000 patients with chronic epilepsy and 3-9 per 1,000 in those with severe, refractory seizures, though its frequency is difficult to calculate. It is most common in patients 20 to 40 years old.
“SUDEP is difficult to detect; it is often unobserved when it happens and autopsy doesn’t reveal any changes,” said William Nobis, M.D., an instructor in the Department of Neurology at Vanderbilt University Medical Center and an expert on SUDEP. “No definitive cause has been discovered, but we believe that respiratory dysfunction leads to cardiac abnormalities and arrest.”
“We have some clues that the pathways involve the amygdala and the brainstem.”
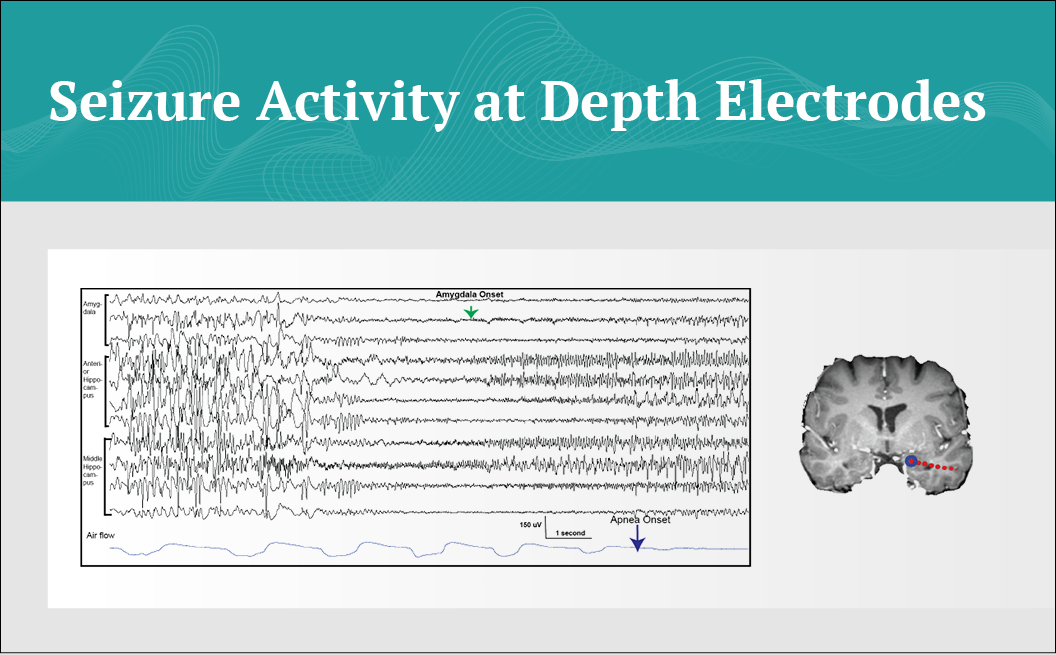
While the brain regions responsible for a seizure’s role in inducing respiratory depression are unclear, “we have some clues that the pathways involve the amygdala and the brainstem,” Nobis said. In a new study published in the Journal of Neurosurgery, Nobis and colleagues at Northwestern University suggest that activation of amygdalar networks is correlated with central apnea during seizures.
Role of the Amygdala
Earlier animal studies had shown Nobis and colleagues that amygdalar networks may influence respiration, leading them to hypothesize the amygdala-brainstem connection. In a 2018 clinical study, they confirmed a functional connection between the amygdala and respiratory control in humans. The results suggested that specific amygdalar nuclei may be critical in mediating this effect.
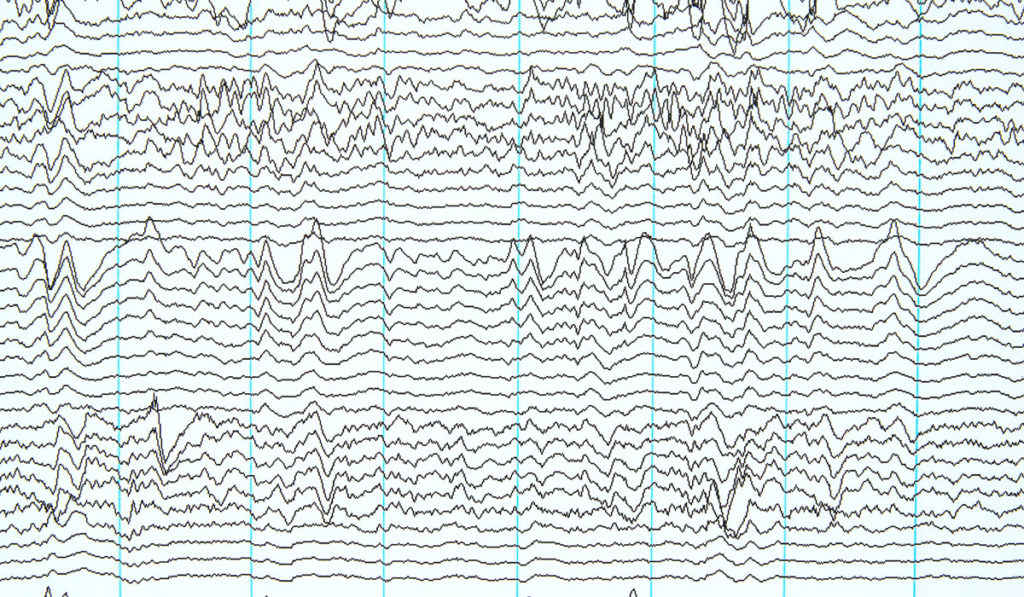
In their latest study, the researchers reviewed all intracranial EEG studies performed at Northwestern Memorial Hospital since 2010 that were accompanied by respiratory monitoring. The goal was to understand the relationship between seizure spread to specific mesial temporal brain regions and the onset of apnea.
Apnea associated with each seizure was highly correlated with seizure spread to the amygdala. Across 22 seizures, onset of apnea occurred 2.7 ± 0.4 (mean ± SEM) seconds after the spread of the seizure to the amygdala, which was significantly earlier than after spread to the hippocampus (10.2 ± 0.7 seconds; p < 0.01).
“The study builds on our prior work that demonstrates a role for the amygdala in voluntary respiratory control and suggests a further role in dysfunctional breathing states seen during seizures,” Nobis said. “We think the results have implications for SUDEP pathophysiology.”
Preventing SUDEP
SUDEP prevention relies on strict disease management. “Right now, the only thing you can do to prevent SUDEP is to control your epilepsy,” Nobis said. “Take your medications; sleep well; don’t use alcohol; manage stress. Basically, don’t do anything that would bring on a seizure.”
The FDA has approved a “smartwatch” device—the Embrace from Empatica—which uses machine-learning to detect possible seizures and immediately notify caregivers through a smartphone app. There is also an app for tracking seizures and monitoring daily rest and physical activity. “Plus, the device looks good; it’s something young people will wear,” Nobis said.
Nobis is working with an interdisciplinary team at Vanderbilt to further explore the amygdala-brainstem circuitry using mouse models, and through translational projects observing epilepsy patients at risk for SUDEP with functional imaging (functional MRI and diffusion tensor imaging).
“It is our hope that by finding this important circuit, we can begin to target neuromodulatory and pharmacologic interventions and other novel approaches to prevent SUDEP.”
“These seizures with apnea are more common than we thought. It is our hope that by finding this important circuit, we can begin to target neuromodulatory and pharmacologic interventions and other novel approaches to prevent SUDEP from occurring,” Nobis said.