Sacral nerve stimulation technology that is benefitting many overactive bladder (OAB) patients is gaining momentum for the treatment of fecal incontinence (FI). FDA-approved for OAB since 1997, Medtronic’s Interstim™, a sacral nerve stimulator implanted in the upper buttock, won approval for fecal incontinence in 2011. The latest version of the device, the smaller Interstim™ Micro, is demonstrating success in Europe since its rollout in January.
Molly Ford, M.D., a colon and rectal surgeon at Vanderbilt University Medical Center, studied the Interstim™ technology in her fellowship and brought the procedure to Vanderbilt in 2014. “Neuromodulator devices were slow to catch on at first, mostly because there are a lot of misconceptions about fecal incontinence,” Ford said. “Many providers think there is nothing to do for FI beyond medical management, sphincter repair — which generally does not have sustained results — or colostomy.”
“Many providers think there is nothing to do for FI beyond medical management, sphincter repair — which generally does not have sustained results — or colostomy.”
Improvements in the design of the newest device include the smaller size, longer battery life of up to 15 years, and leads that allow for full-body 1.5 and 3 Tesla MRI-conditional scans.
Ford expects these improvements to help make the technology available to a broader group of patients.
Identifying Candidates for the Procedure
The primary indication for a sacral nerve stimulator is one or more incidents a week in which there is a loss of bowel control or even significant urgency that requires close proximity to a bathroom. Women are much more likely to have FI due to shorter anal canals and childbirth-related pelvic floor damage and subsequent muscle atrophy. While Ford treats some younger women, most of her patients are 50 and over.
By the time most patients come to Ford and her team, their incontinence has escalated far beyond occasional urgency or leakage to a condition that may even confine them to home. She and her colleagues are seeing 80 percent or more of their patients helped by a sacral nerve stimulation device. “I think they are going back to their primary care or GI doctors and spreading the word that it works,” Ford said.
Therapy Options
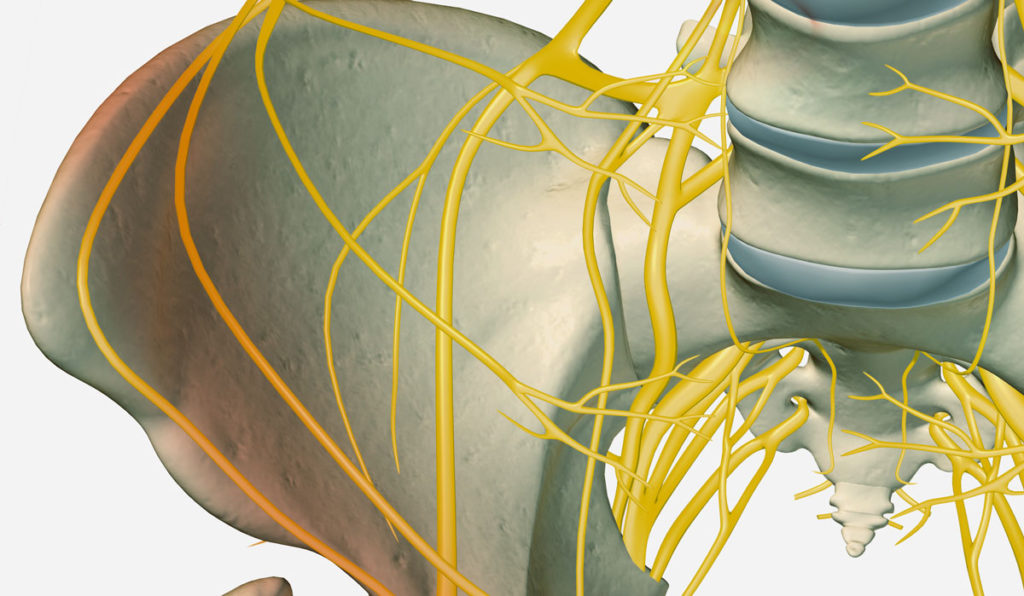
Studies suggest stimulating the sacral complex helps normalize sensory signal processing in the spinal cord. Stimulation is continual, with the patient having some control over the program and the settings. The result is a nerve-based functional change in muscle control. Unlike the case with OAB, where bladder “training” can occur, removing the stimulation generally returns the patient to a state of incontinence.
Since the stimulation works better on some patients than others, office-based tests are necessary to determine who will benefit. First-line therapy for FI is medical management, which includes pelvic floor physical therapy and strengthening exercises, dietary fiber, and Imodium® (assuming no constipation issues). To be a candidate for the sacral nerve stimulator, patients must first “fail” medical management.
Patients who have daily FI episodes may undergo an office-based test where a thin wire is inserted through the lower back into the sacral complex (S3 region) while a portable device worn on a belt delivers stimulation. If improvement is noted after five days, the physician removes the test wire and implants the neuromodulator, Ford explained.
Another option is a two-week test, where the surgeon inserts a tined electrode into the sacral complex and out again to a temporary controller worn on a belt. If the patient experiences a 50 percent or greater improvement over that period, the patient may receive an implant.
Quality of Life Improvements
While Ford says a urologist may perform 20 to 30 OAB implants a year, the rate of implants for FI is lower. This rate is escalating, though, as word spreads about the success rate, defined as a 50 percent reduction in episodes. Many of Ford’s patients have even better results and some are free of FI episodes altogether.
“It’s probably the procedure that makes patients happier than any other procedure I do,” she said. “I have had more people go from truly being a shut-in to functioning in society. I have patients who say, ‘I just want to go to church and have lunch with my friends.’ They come back post-op and they’re back to doing these things and more.”
“It’s probably the procedure that makes patients happier than any other procedure I do.”