In two recently published studies, researchers studied functional magnetic resonance imaging (fMRI) results from a cohort of patients with temporal lobe epilepsy (TLE) to find out how temporal lobe resection affects functional connectivity of brain structures important for cortical activation. The studies are the first to look at brain connectivity of the brainstem and thalamic arousal network one or more years following epilepsy surgery. Results have set the stage for larger studies now underway to measure the impact of surgery on neurocognition and connectivity.
The work was led by principal investigator Dario J. Englot, M.D., surgical director of epilepsy at Vanderbilt University Medical Center, and by first author Hernán González, M.S., graduate student at Vanderbilt University School of Medicine.
Approximately one million Americans have epileptic seizures that are medication-resistant. A majority of these people have TLE, and most are candidates for a surgery that yields a 70 percent seizure cessation rate, with low rates of physical and cognitive side effects. Yet only a few thousand have had this surgery. “It’s one of the most underutilized medical treatments for a major disorder, even though it’s effective,” Englot said.
Seizure Morbidity and Brain Connectivity
Frequent and long-term TLE seizures can have a pervasive impact on neurocognition, gray matter atrophy, and connectivity among brain regions. In prior work with Victoria Morgan, Ph.D., associate professor of radiology at Vanderbilt, the researchers had found patients with TLE have decreased connectivity between brainstem arousal centers and the neocortex compared to healthy control subjects.
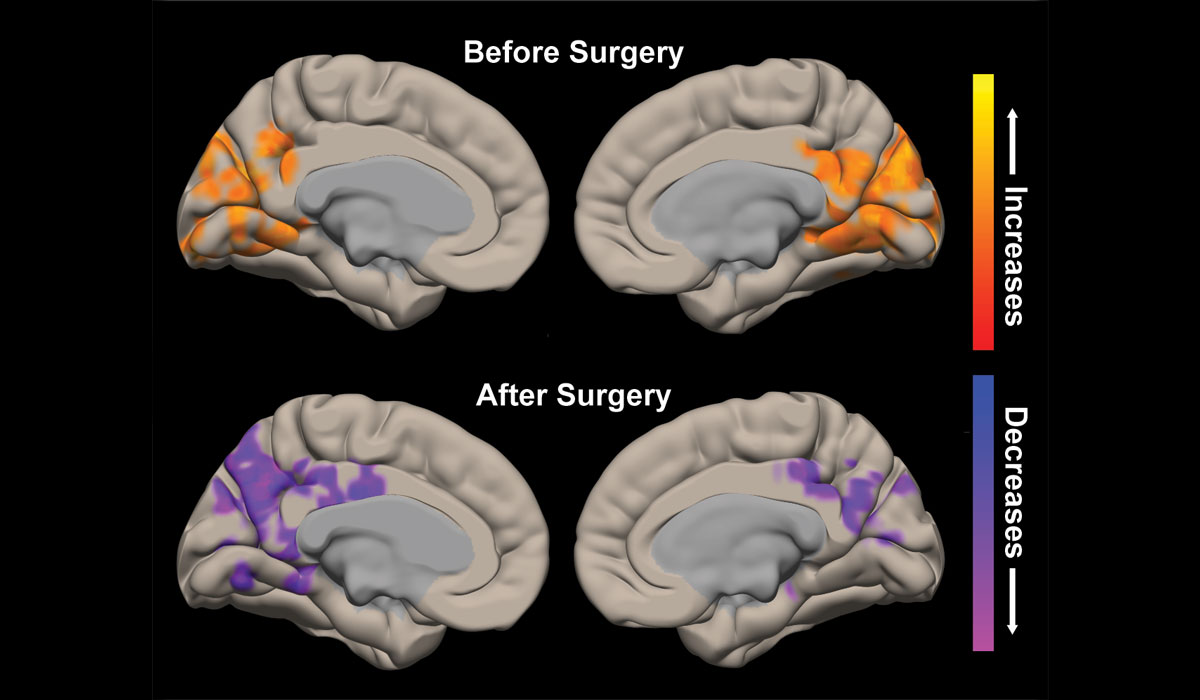
In a Neurosurgery study, the team sought to learn how successful epilepsy surgery impacts arousal centers of the brainstem. They measured and compared the functional and structural connectivity of brainstem ascending reticular activity system structures in 15 adult patients, before and after surgery, and in 15 matched control subjects.
Surgery had rendered 10 of the 15 TLE patients seizure-free, and the remaining five experienced seizure reduction. In the seizure-free patients, the investigators observed improved functional connectivity between brainstem arousal centers and neocortex, but no change in structural connectivity. While all 10 patients experienced improved connectivity, those with the greatest deficits before surgery demonstrated bigger improvements.
“We know that chronic seizures can have a large impact on neural connectivity… what’s surprising is that post-surgery connectivity can improve to levels very similar to healthy control subjects.”
“We know that chronic seizures can have a large impact on neural connectivity, but what’s surprising is that post-surgery connectivity can improve to levels very similar to healthy control subjects,” González said.
In the Journal of Neurology, Neurosurgery & Psychiatry, the authors examined pre- and post-surgical functional connectivity between the thalamic arousal center and both the cortex and brainstem in patients with TLE. Resting state fMRI was performed on 26 patients with TLE and 26 matched controls.
After surgery, 19 patients with reduced seizure frequency showed partial recovery of functional connectivity of the thalamic arousal network, with values more closely resembling controls.
Aiming for Higher Predictive Potential
Englot and his team are now enrolling 25 surgical patients for pre- and post-op neurocognitive assessments. “Until now, we have only looked at some verbal memory and verbal intelligence ratings. This time, we will do a full assessment and follow-up 12 months after surgery,” he says. Comparing fMRI results to test scores will begin to create a composite picture of how connectivity changes manifest as neurocognitive changes.
Many factors that determine surgery success remain largely unknown. Surgeons use scalp or intracranial electrodes to map seizure origination, and if the sources are not known or are traced to an area of the brain that is dangerous to resect, surgery is ruled out.
With TLE, however, safe resection is common. Still, because one-third of surgical patients do not become seizure-free, Morgan and colleagues are conducting a network analysis that will help predict which patients will stop having seizures after surgery.
“By performing these connectivity tests and matching past and prospective patients’ fMRI profiles, we can more readily predict the odds of success and present these to patients and their families,” Englot says.