Caught early, lung cancer cure rates approach 50 percent. Yet, while breast cancer and colorectal screening function with almost clockwork efficiency in many markets, lung cancer screening is in its infancy. The American Thoracic Society and the American Lung Association recently published The Lung Cancer Screening Implementation Guide to help health systems launch, expand and improve lung cancer screening programs. The guide is a product of collaboration among experts from 16 institutions.
Kim L. Sandler, M.D., a cardiothoracic radiologist and co-director of the Vanderbilt Lung Screening Program at Vanderbilt University Medical Center, was a contributing expert to the implementation guide. Sandler says many health systems, including Vanderbilt, have adopted a centralized, streamlined program model for lung cancer screening because of scarcity of time and resources among primary care physicians.
“One of the most common arguments against lung cancer screening is that it puts too much of a burden on referring providers.”
“One of the most common arguments against lung cancer screening is that it puts too much of a burden on referring providers, particularly with the shared decision-making visits, which can be time-consuming,” Sandler says. “In addition, patients have a wide variety of incidental findings, so referring providers may need to not only explain the results of a scan to their patients, but also make next step referral decisions.”
Building a Centralized Model of Care
Both Sandler and pulmonologist Otis Rickman, D.O., serve as co-directors of Vanderbilt’s lung screening program, launched in 2013. Sandler describes the program as “highly centralized.”
“We work with providers on whatever basis they prefer, but over 95 percent have asked that we complete the shared decision-making visit within radiology as part of our screening protocol.”
The program’s clinical coordinator, Alexis Paulson, M.S.N., conducts decision-making visits with patients, discussing the risks and benefits of screening, the possibility of a false positive result, and what other tests may be needed if there is something abnormal.
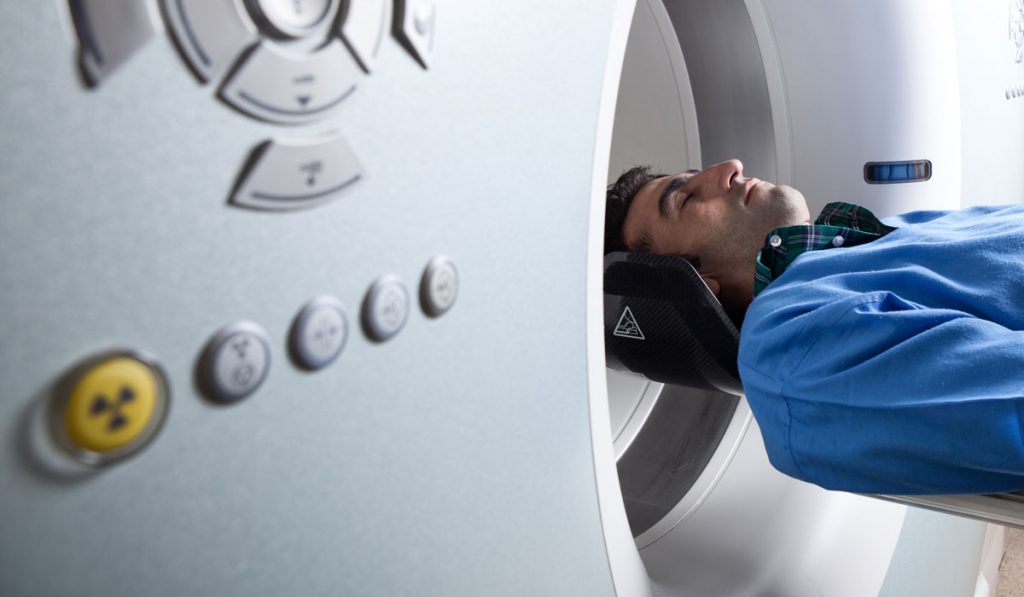
A CT scan is performed immediately following the shared decision-making visit, with results back to the referring physician and the patient in 24 to 48 hours. The 15 percent or so who have an abnormal result can be referred to the lung nodule clinic. “We follow up throughout, making sure the patients keep appointments and have the appropriate studies,” Sandler says.
Paulson is also a certified tobacco treatment specialist and provides smoking cessation counseling for current smokers, repeating this with each screening, since patients are more likely to quit smoking when enrolled in a program. “A patient may not be ready to quit at the time of their initial screening, but with yearly follow-ups, we may talk with them at a later time when they are ready,” Sandler says.
Expanding Lung Cancer Screening
Less than five percent of eligible individuals are screened for lung cancer today, says Sandler, yet the urgency is clear. In Vanderbilt’s program, while over three percent of screened patients are found to have cancer, approximately 70 percent of these patients have had treatable early stage disease.
Sandler is working to extend screening across the Vanderbilt Health Affiliated Network. “We are starting to put together a care path so that other hospitals within the network can look to what we’ve done and establish their own programs.”
The CDC offers guidance for institutions looking to start a new lung cancer screening program. In general, Sandler places these among the key elements that make a program succeed:
- A centralized program model, or a hybrid between centralized and decentralized that includes easy access to referral resources.
- Shared decision-making and smoking cessation counseling.
- Adequate professional staff to cover the necessary disciples and provide the counseling.
- A strong marketing focus, necessary to reach into pockets of society where people are unaware of lung screening.
- Availability of lung screening consultation appointments, preferably on the same day as primary care visits.
Vanderbilt’s program has grown from 200 patients screened in 2015 to over 1,500 today. Sandler hopes to expand the program so that there is a walk-in screening opportunity. “I’d love to see us in five years have as many as 5,000 patients in the program, if not more,” she says.