Transurethral resection of the prostate (TURP) has long been considered the gold standard surgical therapy for lower urinary tract symptoms resulting from benign prostatic hyperplasia (BPH) and bladder outlet obstruction. Today, minimally invasive surgical treatments and laser therapies are challenging TURP, and one of leading contenders is Holmium laser enucleation of the prostate (HoLEP).
HoLEP has been used worldwide to treat BPH and numerous randomized controlled trials have shown its superiority to traditional surgical approaches. Earlier this year, in its updated surgical BPH guidelines, the American Urological Association recognized HoLEP as the only treatment recommended to treat prostates of any size. Despite level one evidence for HoLEP and its recommendation by the AUA, a recent study reported HoLEP constitutes only 4% of all BPH operations in the United States.
“As physicians, we always believe that evidence-based medicine is going to change practice, and this is one of those procedures we really have the evidence for,” said Nicole Miller, M.D., associate professor of urology at Vanderbilt University Medical Center. “However, in this case the evidence has not been enough. HoLEP has essentially remained confined to a select number of high volume referral centers.”
Patients Requesting HoLEP
Miller said the learning curve is the issue; the procedure requires significant technical expertise. Another factor is that reimbursement has not kept up with the effort and training required. However, demand is now coming from the patient side. Vanderbilt has been offering HoLEP since 2008 and is one of the top centers in the U.S., performing 200 to 250 procedures annually.
“Today, HoLEP constitutes 80 percent of my practice,” Miller said. “Patients are educating themselves and finding us online. They want to alleviate their urinary symptoms and they want to do it one time. You can remove much more tissue with this surgery and the better we relieve the prostatic obstruction, the better the outcome.”
Surgical Advantages of HoLEP
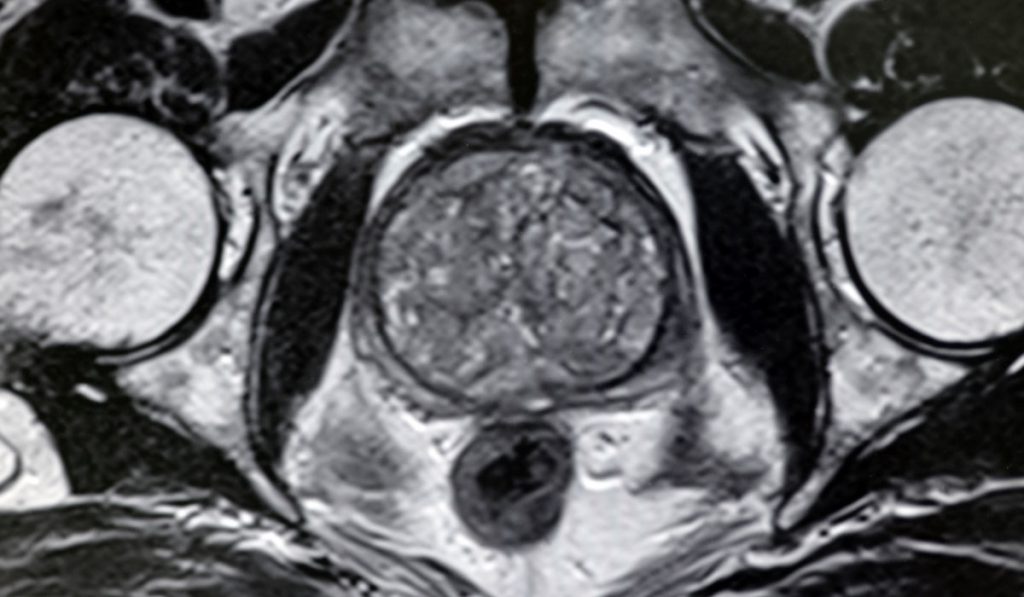
HoLEP requires no incision. A rigid scope goes through the urethra and the surgeon uses a Holmium laser to get into the space between the enlarged prostate tissue transitional tissue and the outer portion of the prostate. Coagulating features of the laser lower transfusion rates from 18 percent for open surgery to less than 4 percent for HoLEP, making it an ideal procedure for resecting large adenomas.
HoLEP can be applied to the majority of patients regardless of prostate size, previous operations, or the condition of the bladder muscle. HoLEP can also be carefully considered in patients requiring anticoagulation or who are undergoing active surveillance for low-risk prostate cancer. Immediate complication rate is low and incontinence is rare, Miller says. And the retreatment rate for HoLEP is lower than reported for other endoscopic BPH procedures.
“While there are still clinical scenarios where incision surgery is indicated as the initial intervention, HoLEP is highly effective in the surgical management of conditions caused by BPH,” Miller said. “Even when comparing HoLEP to robotic simple prostatectomy, there remains a real benefit to HoLEP in its ability to utilize natural orifice surgery.”
“When a patient has had this surgery, PSA drops 70 to 80 percent and becomes a much better marker for diagnosing prostate cancer.”
HoLEP and Prostate Cancer
Because HoLEP resects the prostate from the inside out, a morcellator can be used to remove large pieces of prostate that remain in the bladder. This enables the surgeon to maintain the integrity of the tissue in order to examine it for malignancy.
“We find 9 to 10 percent incidental prostate cancers; the majority of which ultimately observed on active surveillance protocols,” Miller said, “but there is nothing about this procedure that precludes a patient from having prostate cancer treatment. HoLEP doesn’t prevent cancer, but in my experience when a patient has had this surgery, PSA drops 70 to 80 percent and becomes a much better marker for diagnosing prostate cancer; you’re taking out the background noise.”