New research has parsed out pathologic differences between young and old patients with chronic sinusitis (CRS), uncovering marked differences in mucus characteristics and tissue signatures. The findings help to explain the chronic nature of older CRS patients’ inflammatory processes and may lead to novel or redirected therapies to treat them. Findings may also inform the choice between corticosteroid and antibiotic therapies for other age-related conditions.
In the Journal of Allergy and Clinical Immunology, researchers identified a unique immunologic/inflammatory signature in adults over 60 with CRS, characterized by higher levels of pro-inflammatory cytokines in the mucus and persistent issues with bacterial colonization (due to a poor immune response to foreign antigens and pathogens). While corticosteroids and standard antibiotics are the first-line of therapy for patients with CRS, an older immune system is often unable to sustain a durable cure.
Justin Turner, M.D., an otolaryngologist with Vanderbilt University Medical Center and co-author of the study, has seen firsthand the suffering and frustration of chronic CRS patients, as well as the economic burden CRS brings to healthcare systems. “This study helps point us in a better direction,” Turner said. “Currently, disease management is not tailored to age or other demographic factors. This study indicates we should rethink this.”
Distinct Inflammatory Responses Between Young and Old
Mucus samples from the middle meatus or ethmoid cavity were collected from 147 study patients with diffuse, inflammatory CRS who were undergoing endoscopic sinus surgery following failure of other treatment. Thirty control patients were undergoing surgery for other indications and did not have a history of CRS. Patients spanned an age range of 18 to 70.
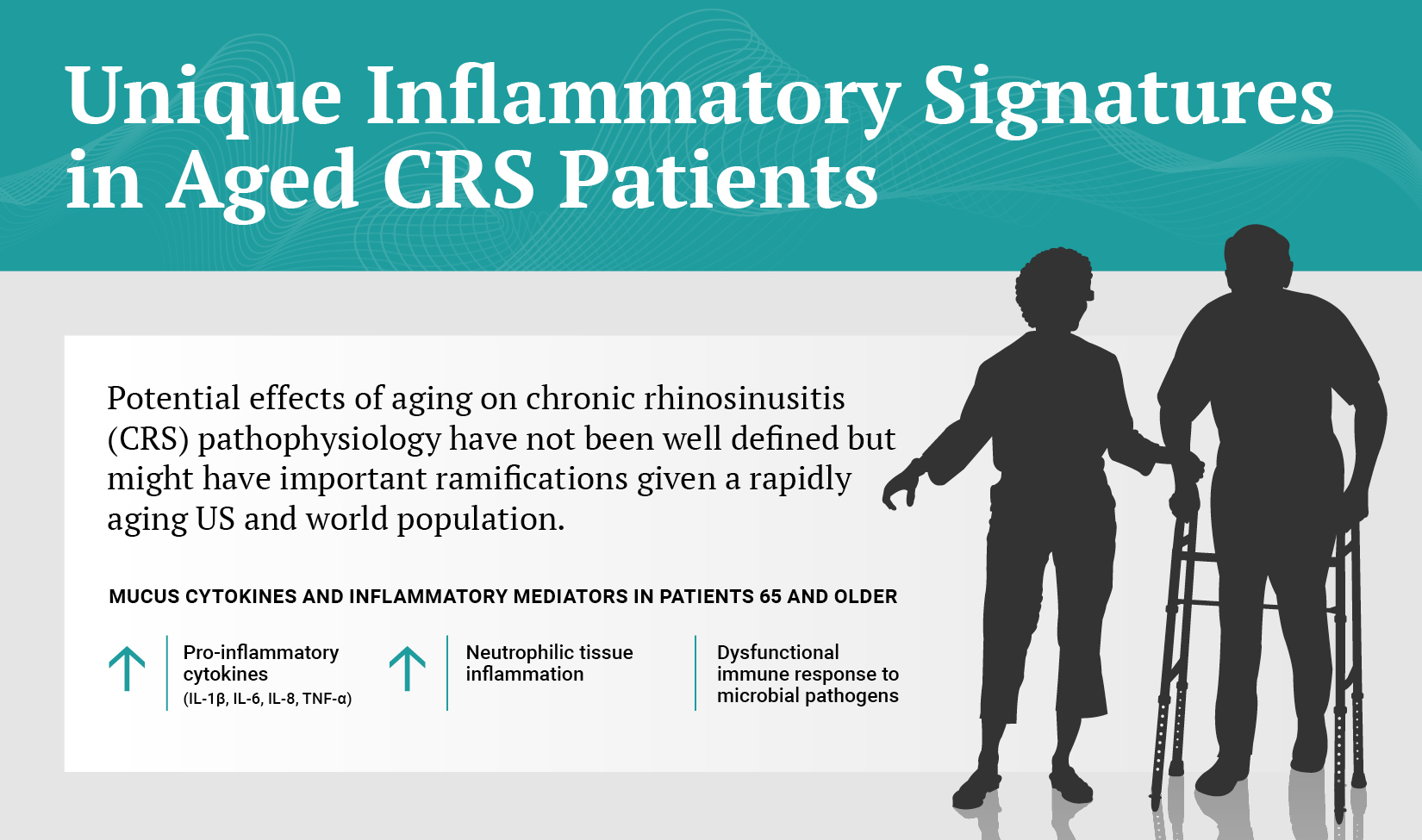
The researchers measured levels of 17 mucus cytokines and inflammatory markers. The study sought to “characterize inflammatory CRS endotypes and determine whether age was associated with specific immune signatures,” wrote the authors.
Patients over 65 in both cohorts had higher levels of neutrophilic tissue inflammation and bacterial colonization or infection. They also had elevated levels of specific pro-inflammatory cytokines commonly associated with the body’s innate immune response, including IL-1-β, IL-6, IL-8, and TNF-α, as compared to younger patients.
“This study confirmed that older patients have higher levels of neutrophils and lower levels of eosinophils.”
“We know that these cytokines are frequently associated with neutrophilic rather than eosinophilic tissue inflammation,” Turner said. “This study confirmed that older patients have higher levels of neutrophils and lower levels of eosinophils.” The findings help explain why treatment used across the board may be missing the mark for older patients, Turner says.
A New Angle on Therapy
Treatment for CRS typically includes oral antibiotics, topical and systemic corticosteroids and surgery. Identifying the age-related differences may point away from the use of corticosteroids, which preferentially target eosinophilic inflammation, and toward use of antibiotics like macrolides that are known to have anti-inflammatory effects in addition to their antibiotic properties. “Ideally, these patients would also be given a drug that augments their immune response to pathogens and antigens or that modifies the activity of specific pro-inflammatory cytokines,” Turner said.
In this era of emerging, if still largely aspirational, personalized medicine, delineating characteristics of specific groups and subgroups is often a stepping stone. Justin Morse, M.D., first author of the study and otolaryngology-head and neck surgery resident at Vanderbilt looks forward to additional research to further delineate the CRS signature in this group.
“All patients can not all be treated uniformly.”
“I hope the findings of this novel endotype within the heterogenous CRS population will be a catalyst to not only further investigate these patients but also to reshape how we, as clinicians, treat this specific group. We realize all patients can not all be treated uniformly,” Morse said.





