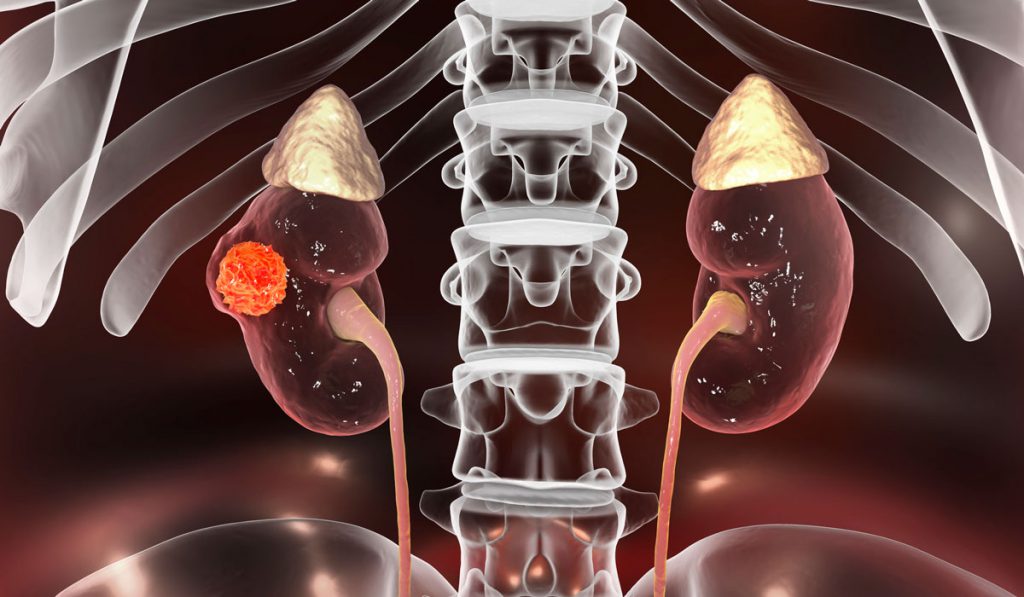
Kidney cancer is one of the more successfully treated cancers. Caught early, five-year survival rates are 75 percent, although they range from 12 percent (following metastasis) to 93 percent (when cancer remains localized in the kidney). Unfortunately, patients with non-clear cell renal cell carcinoma (nccRCC), who constitute about 20 percent of renal cancer patients, generally respond more poorly to therapy.
Despite the fact that nccRCC tumors have unique biologies and respond differently to therapy, treatment has remained essentially uniform for all histologic types of kidney cancer. At the American Urologic Association conference in May 2019, Nancy B. Davis, M.D., genitourinary oncologist at Vanderbilt University Medical Center, addressed the growing recognition of the unique characteristics of nccRCC. “At one time, we thought kidney cancer was kidney cancer. Now we know that’s just not true,” Davis said.
“nccRCC tumors don’t look or behave like ccRCC at all.”
Recognition that not all patients respond similarly to treatments is leading to more research into what nccRCC tumors really look like, including their histology and molecular features, and growth patterns. “nccRCC tumors don’t look or behave like ccRCC at all,” Davis says, “not histologically, and more importantly, not biologically.”
Unique Histology and Therapies for nccRCC
The 20 percent of cases classified as nccRCC are further subdivided; the papillary and pchromophobic subtypes represent about 10 to 15 percent of non-clear cell kidney cancer, with a number of other variations, at under one percent each, composing the remainder. There may also be clear cell and non-clear cells in the same tumor, further complicating diagnosis and treatment. “You can have a clear cell carcinoma that has sarcomatoid or other non-clear cell features. Depending on the ratio, the tumor will act more like one or the other,” Davis says.
Modern immunotherapy has become the standard of care in clear cell renal cell cancers, but it remains to be seen if these treatments will be as successful in the nccRCC histologies. “We really don’t know yet, because it is difficult to aggregate enough patients, particularly with the more rare nccRCC, to constitute a study group,” Davis said.
Davis urges greater inclusion of nccRCC patients as subgroups in larger trials. Current trials, like KEYNOTE-427 (an ongoing trial evaluating single agent pembrolizumab for tumor shrinkage), are accruing nccRCC cohorts, though most don’t specify the type of nccRCC. The recently reported objective response rate for the nccRCC cohort in KEYNOTE-427 is around 25 percent, with 5 percent experiencing complete responses. This is lower response than seen in the ccRCC cohort, but higher by historical comparison.
Results from other trials revealing differences in objective response rates between nccRCC subtypes underscore the need to recognize individual signatures.
Next Gen Sequencing May Yield Better Therapies
Next generation sequencing may be the most promising pathway for treating esoteric variants of nccRCC and other cancers. By evaluating the somatic mutations of an individual patient’s tumor tissue, sequencing may identify a drug that targets the particular receptors found on that patient’s tumor. “It’s not formulaic, it’s truly personalized medicine, and what might most benefit patients with nccRRC,” Davis says.
MATCH, an ongoing trial with multiple arms, is looking at genetic screening across cancers. But until this technology develops commercially, clinical research on nccRCC treatment may continue mostly as add-on cohorts to ccRCC trials.
“We know that patients with nccRCC do not respond as well to our typical therapies for kidney cancer, so we need to find better, more effective therapies for this subgroup,” Davis said. “In the meantime, we have to recognize that we have a unique population and a difficult algorithm to solve.”