Cerebrovascular changes, including small vessel disease (SVD), contribute to more than 80 percent of all autopsy-confirmed cases of dementia and are the most common pathology to co-occur with Alzheimer’s disease. Enlarged perivascular spaces (PVS), a form of SVD, have long been considered a benign neuroimaging feature in older adults. Now, a landmark study published in Neurology has found that PVS may have important associations with cognitive performance, particularly information processing speed and executive function.
The study, which looked at older adults without dementia, offers evidence that SVD is not a singular construct. Rather, it is likely a diverse mechanism in which multiple neuroimaging markers reflect distinct pathways of injury, as well as early or late features of severity.
“Enlarged perivascular spaces contributed to adverse cognitive health through a unique pathway of injury that was distinct from the other markers.”
“Enlarged perivascular spaces contributed to adverse cognitive health through a unique pathway of injury that was distinct from the other markers,” said senior author Angela L. Jefferson, Ph.D., professor of neurology and director of the Vanderbilt Memory and Alzheimer’s Center at Vanderbilt University Medical Center. “That result was unexpected and emphasizes that enlarged perivascular spaces deserve further study. Our work shows they are not clinically insignificant.”
Comparing PVS with Other Markers
The PVS study was designed to relate multiple SVD neuroimaging markers to cognition in older adults. The study used data from the Vanderbilt Memory & Aging Project (VMAP), a longitudinal investigation of vascular health and brain aging. Launched in 2012, the VMAP cohort includes 335 community-dwelling participants age 60 to 92, including 168 individuals with mild cognitive impairment and 167 cognitively unimpaired adults.
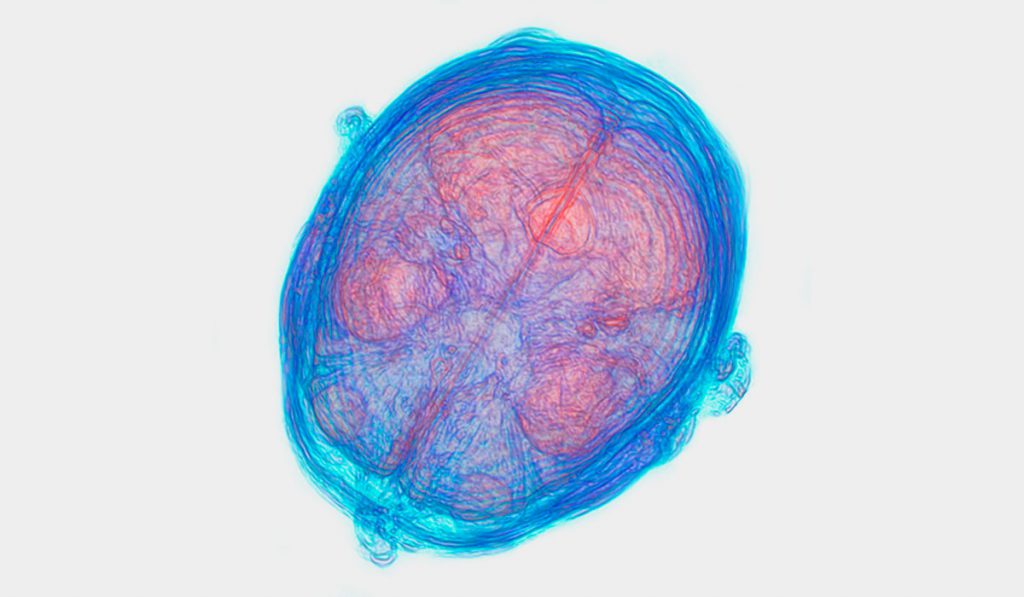
In the PVS study, 327 VMAP participants free of clinical dementia and stroke (age 73 ± 7 years, 59 percent male, 40 percent with mild cognitive impairment) completed neuropsychological assessment and 3T magnetic resonance imaging to measure white matter hyperintensities (WMH), PVS, cerebral microbleeds (CMBs), and lacunes. Linear regressions related each SVD marker to neuropsychological performance and adjusted for age, sex, race/ethnicity, education, cognitive diagnosis, apolipoprotein E ε4 presence (a genetic risk factor for Alzheimer’s disease), Framingham Stroke Risk Profile, and intracranial volume.
Uncovering New Biomarkers
The authors looked at each of the neuroimaging markers to determine if they related to different cognitive activities, such as language, memory, visuospatial skills, information processing speed and executive function, and if the markers reflected a common or unique pathway of injury.
In comparison with common markers of SVD, results showed a more frequent association between enlarged PVS and cognition than expected. And while some SVD markers overlap in connection to cognition, PVS correlated with distinct injury pathways.
WMH related to the most neuropsychological measures, including language, information processing speed, executive function, and visuospatial performances. The next most frequent links were between enlarged PVS and both information processing speed and executive function performances. Lacunes and CMBs related to fewer measures than expected. Combined models simultaneously testing multiple statistically significant SVD predictors suggested that WMH, PVS, and CMBs each independently correlated with information processing and executive function performances; however, compared to other SVD markers, PVS remained statistically significant related to information processing and executive function performances.
“These results are important for any clinician or scientist who works in aging.”
“These results are important for any clinician or scientist who works in aging,” said Jefferson. “Many of these small vessel disease markers are due to common vascular risk factors for cardiovascular disease, such as high blood pressure or diabetes. We know these conditions can be prevented and treated, which means small vessel disease and its impact on abnormal cognitive changes can be prevented.”
This research was funded by the Alzheimer’s Association, the National Institute on Aging, the National Institute of Neurological Disorders and Stroke, the Vanderbilt Clinical Translational Science Award, and the Vanderbilt Memory & Alzheimer’s Center.