Peripheral artery disease (PAD) affects over 8.5 million people in the U.S. and 12-20 percent of people over 60. With diabetes incidence climbing, PAD threatens mobility and lower limb integrity for a growing number of people.
Each year, clinicians perform about 83 graft and 584 endovascular procedures per 100,000 Medicare patients to revascularize lower limbs. A significant percentage of these procedures fail in the first year, leading to second, more complicated surgeries and worse prognoses. The options when a second procedure fails are sparse—last resort amputation affects over two million adults in the U.S. today.
Under NIH and AHA grants, Joshua Beckman, M.D., director of vascular medicine at Vanderbilt University Medical Center, is coordinating two multipronged, multicenter research studies of microvascular architecture, muscle metabolism and genetic profiles to help elucidate how PAD develops and who is most at risk.
“I’m hopeful that by the end of these grants we can tell clinicians, first, ‘These people are at high risk for PAD and you should check them out to see if they have it,’ and second, ‘This is the subset of people most likely to go on and have severe problems with it,” Beckman said.
Platelet Function and Graft and Stent Failure
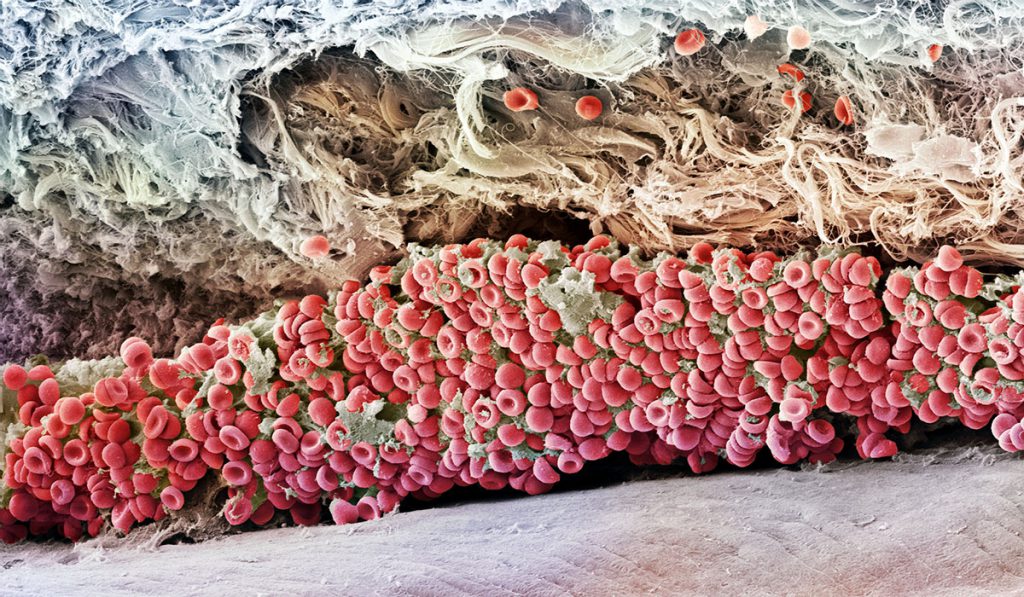
The investigators will study critical limb ischemia at a molecular level, with the goal of clarifying why some bypass graft and endovascular (angioplasty and stent) procedures fail and which procedures are superior.
Vanderbilt’s substudy within the NIH Best Endovascular vs. Best Surgical Therapy in Patients with Critical Limb Ischemia (BEST-CLI) trial focuses on how diabetes and platelet overactivation affects outcomes with stents and bypass grafts. “Patients with diabetes suffer a disproportionate number of amputations. This work will begin to shed light on the worse prognosis in these patients,” Beckman said.
To explore platelet function, Olivier Boutaud, Ph.D., a Vanderbilt researcher in pharmacology, developed a way to “freeze” platelet activity so that platelet samples could be extracted, packaged and mailed overnight in an unaltered state. Forty centers are now sending samples from PAD patients to Vanderbilt, and Boutaud is assessing how the level of platelet activation in these samples correlates with clinical outcomes.
Multifaceted Research Into Lower Extremity Dysfunction
Through an American Heart Association Strategically-focused Research Network grant, Vanderbilt investigators and colleagues are also studying differences in how lower extremity muscles and blood vessels function, on a molecular and microvascular level, in patients with and without PAD. Key research questions are:
1. How do leg muscles get the energy and nutrients they need? Since poor muscle function is connected with PAD, what goes wrong in this process?
David Wasserman, Ph.D., who heads Vanderbilt’s Department of Molecular Physics and Biophysics, is studying at the smallest blood vessel level the mechanisms for how insulin, glucose and other nutrients enter muscle cells.
2. What happens to blood vessel function, calf muscle architecture and function, blood
metabolism and acid accumulation when blood flow is arrested in people with and without PAD? What happens when revascularization takes place?
Beckman is working with Manus Donahue, Ph.D., at the Vanderbilt University Imaging Science Institute and Rob Gerszten, M.D., at Beth Israel Deaconess Medical Center to study MRI images acquired during exercise simulation and at rest.
“This will help us understand what is happening in the blood vessels and the muscles in response to PAD, revascularization with surgery or stent fixes. We hope to target the abnormalities, see how our interventions reduce the dysfunction, and try to find therapies to reverse these responses,” Beckman said.
3. Can genetic profiles tell us who is at risk for developing PAD and who will suffer from PAD-related morbidity?
Matt Freiberg, M.D., and Quinn Wells, Pharm.D., both of Vanderbilt’s Division of Cardiovascular Medicine, are using electronic health record data from 4.3 million veterans, including 500,000 with genetic profiles, to examine the epidemiology and genetics of PAD.
Making the Case for Screening
“Even if third party payers think we shouldn’t screen all adults, I hope our research will clearly point to the need for screening all those who might benefit.”
The CDC reports that up to 40% of individuals with PAD experience no leg pain, leaving many undiagnosed. Beckman said that identifying the at-risk population is key, but there are barriers to screening that he hopes their research could help lower.
“A simple ankle-brachial index screening, though one of the least expensive tests there is, is not covered in four out of the seven Medicare zones unless the patient complains of difficult or painful walking,” he said. “Even if third party payers think we shouldn’t screen all adults, I hope our research will clearly point to the need for screening all those who might benefit.”