With an incidence of just 1.2 in 100,000, vagal schwannomas have not had the spotlight needed to attract research or support specific surgical training in their removal. They are, however, a shining example of how patients with rare conditions can rally to find specialists and treatments that can radically impact outcomes.
James Netterville, M.D., associate director of the Bill Wilkerson Center for Otolaryngology and Communications Sciences at Vanderbilt University Medical Center is one of few surgeons in the world experienced in schwannoma enucleation—a neural function-sparing technique used as an alternative to standard resection. Preserving normal function of the vagal nerve is critical to maintaining use of muscles in the face, shoulder or arms.
In 2013, a 60-member online support group that included some of Netterville’s patients asked him to join as medical advisor. Today, the 600-plus member group is thriving, and Netterville has become a resource and conduit for schwannoma patients worldwide.
“This group is by far the largest ‘database’ of head and neck schwannomas that has ever existed.”
“This group is by far the largest ‘database’ of head and neck schwannomas that has ever existed, so the learning potential it offers may unbelievably enhance our ability to improve care,” Netterville said.
Challenges in Schwannoma Removal
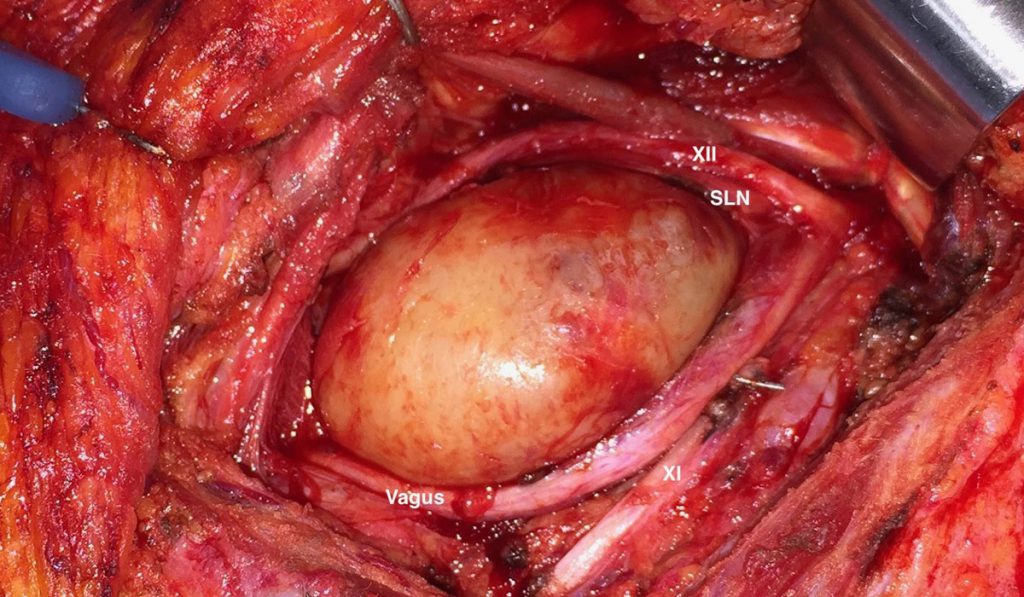
Schwann cells are insulators that form the myelin sheath around axons, protecting nerves and keeping them from cross-communicating. In the head and neck region, schwannomas often reside on the facial, vagus, hypoglossal, or sympathetic nerves, as well as on the cervical and brachial plexus.
When a schwannoma develops, axons are pushed outward to form a web-like network around the tumor and barring easy surgical access. Radiation is sometimes effective if the tumor is small, but often the tumor needs to be resected, causing significant collateral damage to nerve function.
Enucleation as an Alternative Approach
Netterville offers a different option. “I encountered my first large vagal schwannoma 30 years ago, when a Vanderbilt college student came to see me about a lump in her neck,” he said. “I was dismayed at the prospect of nerve damage from resection, so I called a senior head and neck surgeon I admired, who introduced me to the enucleation approach.”
Enucleation protects unseen nerve fibers connected to the vagal nerve. It is a nuanced procedure in which success depends on experience, tumor location and the landscape of the fibers around the tumor. It requires finding or developing a plane between nerve fibers, delicately peeling the nerves back and dissecting the tumor through this narrow window.
“The surrounding critical nerves, including the nerve to the shoulder, the nerves that controls swallowing, and the nerve to the tongue, have intimate connections with the vagus nerve. If I had to cut out the tumor with resection of the entire vagus nerve, I would likely damage the rest of these nerves,” Netterville said.
Enucleation can spare adjacent nerve function and preserve normal voice about 90 percent of the time. “In cases where there is nerve impairment, the patient may have a degree of paresis, but rarely paralysis.”
An Online Patient Community
At the time Netterville joined the online support group, he was skeptical about social media as a positive resource for patients seeking care.
“In the first week, I ended up spending hours each night answering online questions, which became unsustainable. So I uploaded some videos about enucleation and told my patients who monitor the site, if they see someone I could help, give them my contact information,” Netterville said.
As a result of referrals from the group, instead of seeing two to three schwannoma patients a year, Netterville sees that many in a month. He also refers patients to the few surgeons in the U.S. who are gaining experience in this technique.
“I communicate with patients all over the world. We’ll do an iPhone chat, they’ll share their X-rays, and I’ll give them my best advice. I try to help them find someone in their own country or region who does enucleation procedures, but it can be frustrating to find excellent care for them,” he said. Due to this scarcity, he has had patients and their families fly in from Australia, Saudi Arabia and Japan for procedures.
“We all understand that misinformation is rampant on the web. But it’s also amazing to see how many highly intellectual, thoughtful people are getting quality healthcare information this way.”
“Social media is now a major source of healthcare information for patients,” Netterville said. “We all understand that misinformation is rampant on the web. But it’s also amazing to see how many highly intellectual, thoughtful people are getting quality healthcare information this way.”