Psychotic disorders are accompanied by accelerated aging across biologic systems, including the brain. Researchers have associated psychotic disorders with a sharp decline in brain gray matter volume and white matter integrity. However, few have delved into specific cognitive networks affected and their interconnectivity.
Julia Sheffield, Ph.D., postdoctoral fellow in the Department of Psychiatry and Behavioral Sciences at Vanderbilt University Medical Center, recently investigated how brain regions most vulnerable to aging function in people with schizophrenia and bipolar disorder. Sheffield sought to understand how networks connecting the regions aged as psychosis progressed—with the ultimate goal of identifying opportunities for intervention.
fMRI Reveals Networks Affected by Psychosis
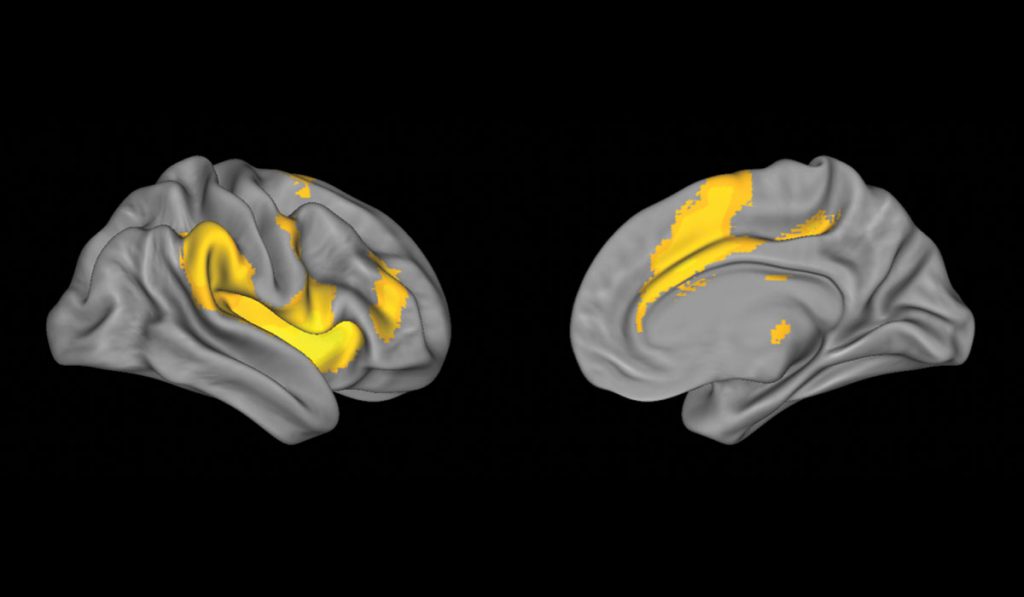
In a study published in Biological Psychiatry, Sheffield and a team of neuroscientists collected fMRI data from 240 adult patients with symptomatic schizophrenia or bipolar disorder type 1, including 110 in the earliest stages of psychosis. They focused on cingulo-opercular network (CON) and frontoparietal network (FPN) interconnectivity, which supports domain-general cognitive ability.
The researchers compared the images to those of 178 age-matched controls. They found the networks were intact in patients with early-stage psychosis, but rapidly declined in patients with chronic psychosis. The declines were consistent with accelerated aging.
Both FPN and CON efficiency declined across all study participants as age increased—and correlated with performance decline on cognitive tests. These effects were more rapid in participants with chronic psychosis.
Opportunities for Intervention
“Even though a patient may have a diagnosis of a psychotic disorder, we can still intervene early to help maintain their brain’s health.”
Although connectivity between the networks declined during disease progression, intact FPNs and CONs during the early stages of psychosis suggest a therapeutic opportunity. Said Sheffield, “This study demonstrates that even though a patient may have a diagnosis of a psychotic disorder, we can still intervene early to help maintain their brain’s health.”
And, other networks remain intact during psychosis, according to the new study. Accelerated aging was not observed in either the subcortical or visual networks in patients with demonstrated psychosis.
The results confirm those of a previous, smaller cohort where Sheffield and colleagues showed functional network efficiency of the CON and FPN declined at an accelerated rate in 46 schizophrenic patients—but not until the disease was considered chronic. Combined, the studies are good news for patients and caregivers impacted by psychotic disorders.
“Patients in the early stages of psychosis have hope that their cognitive ability doesn’t have to decline to the degree we’ve historically seen in chronic patients,” Sheffield said. “That’s exciting, because schizophrenia is often seen as a disease that can’t be easily overcome. Being able to tell patients and families that the patient’s brain is healthier than we would’ve initially thought and providing them with tools to continue on that trajectory gives them hope.”