IMpassion130, a phase 3 randomized trial of women with metastatic triple-negative breast cancer, demonstrated that patients live longer if they receive a combination of immunotherapy (atezolizumab) and chemotherapy (nab-paclitaxel).
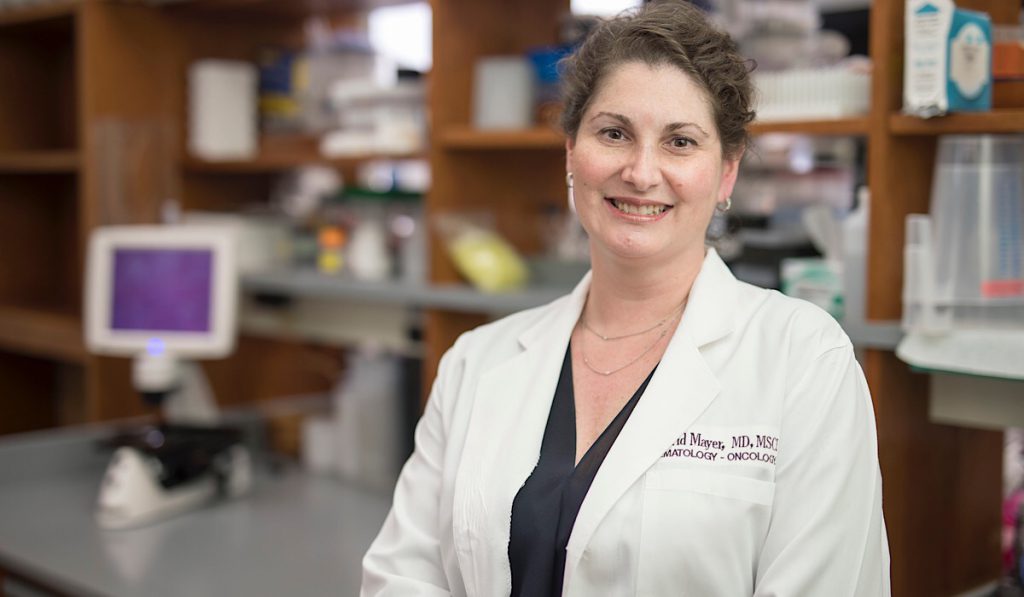
“These findings are very significant for the use of immunotherapy in invasive breast cancers,” said Ingrid Mayer, M.D., director of breast medical oncology at Vanderbilt-Ingram Cancer Center. Mayer believes that combination therapy could provide a realistic chance of prolonged survival in a substantial proportion of patients.
“In some disease, like melanoma, highly active immunotherapy combinations have produced resolution of metastatic disease, with some patients remaining cancer-free after more than a decade,” Mayer said. “We hope this will be the case in patients suffering from metastatic breast cancer.” Mayer and colleagues at Vanderbilt are part of several multi-site trials testing immunotherapy approaches.
(Note: In March 2019, the U.S. Food and Drug Administration granted accelerated approval to atezolizumab (Tecentriq, Genentech/Roche), plus the chemotherapy nab-paclitaxel (Abraxane, Celgene) for the first-line treatment of unresectable locally advanced or metastatic, PD-L1-positive triple-negative breast cancer.)
Immunotherapy in Early HR+/HER2 Cancer
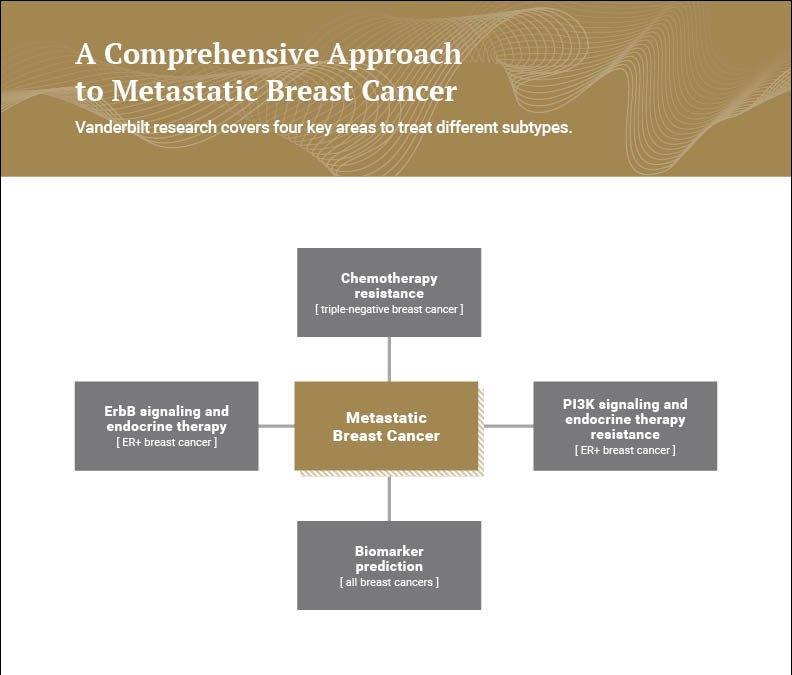
Mayer was principal investigator in the phase 2 NEO-ORB trial, published this month in Clinical Cancer Research. The study explored the use of targeted treatments in early HR+/HER2-negative disease. Genetic alterations of the PI3K pathway, including PIK3CA, are common in HR+ breast cancer and have been linked to endocrine therapy resistance. Additional evidence from the SOLAR-1 study of HR+/HER2 suggested that adding the PI3K inhibitor alpelisib to endocrine therapy (letrozole or fulvestrant) led to improved clinical outcomes in advanced metastatic breast cancer.
NEO-ORB demonstrated that in contrast to the initial results in advanced metastatic disease, addition of alpelisib to 24-week neoadjuvant letrozole treatment did not improve response in patients with HR+ early disease.
“By conducting these clinical trials in patients with operable breast cancer, we hope to identify cancers that do not require chemotherapy.”
“We knew this combination worked in advanced HR+,” Mayer said, “but in our study we discovered that it does not apply to early-stage disease. By conducting these clinical trials in patients with operable breast cancer, we hope to identify cancers that do not require chemotherapy. Our primary aim is to prolong life through treatments that are less toxic.”
Unmasking Tumors to the Immune System
Mayer’s latest research includes trials studying the effect of combination drug therapies in metastatic estrogen receptor-positive (ER+), endocrine therapy-refractory breast cancer and metastatic triple-negative breast cancer (TNBC) patients. The benefits could include a highly active therapy (without traditional chemotherapy) that increases overall survival, and possibly even cure rates in metastatic disease.
One of the drugs contains an anti-PD-L1 antibody known to work in 10-20 percent of patients; the second is a MEK inhibitor. Mayer believes the antibody will help ‘unmask’ the tumor to the immune system and make the immunotherapy drug work better in a greater percentage of patients. “A unifying dogma is that estrogen-positive cancers are immunotherapy ‘cold,’” she said. “We’re hoping to prime the cancer to be more responsive.”
Overall, the trials could help develop both predictive biomarkers of response and early (on-treatment) biomarkers of response, and with additional laboratory research, determine why some patients respond better than others. The investigators also hope to develop imaging techniques that will allow them to observe the immune system’s reaction to the drugs without the need for biopsy.
The trial for patients with ER+ metastatic breast cancer is one of 10 projects launched by Stand Up to Cancer (SU2C) and the American Association for Cancer Research. The SU2C Catalyst clinical trial program is enabling researchers from more than 30 institutions to collaborate across academic and corporate borders on a variety of cancers.