Following a promising Dutch study published in 2018, use of hyperthermic intraperitoneal chemotherapy (HIPEC) as part of a multi-stage treatment protocol is raising some hopes for extending survival and improving cure rates for women with advanced ovarian cancer.
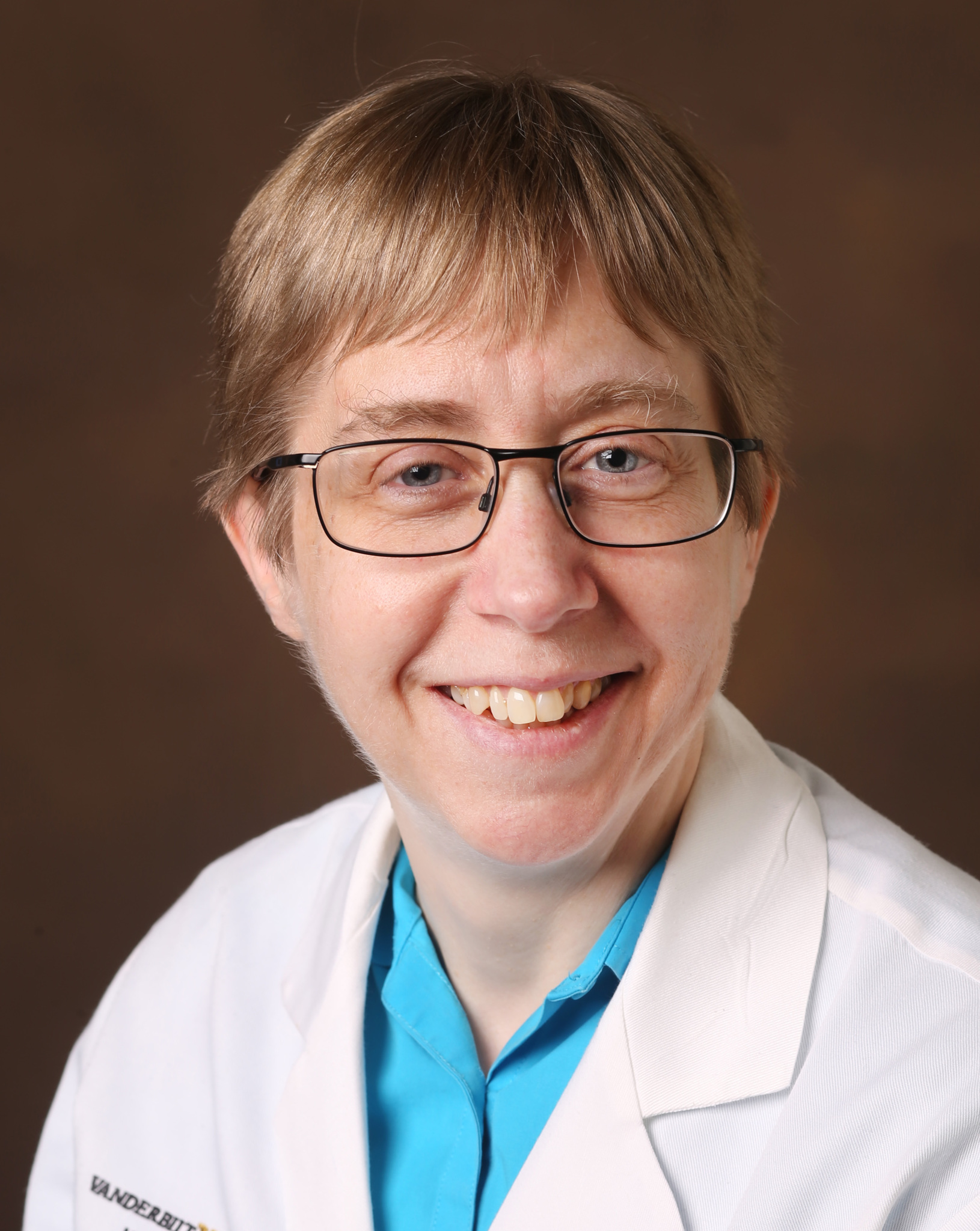
“We are all looking for the holy grail, the treatment that knocks out all the cancer cells,” said Marta Crispens, M.D., director of gynecologic oncology at Vanderbilt University Medical Center. “What is interesting about the van Driel [Dutch] study is their success with longer patient survival. Whether it is HIPEC that makes that difference or HIPEC in conjunction with a specific treatment regimen, we certainly want to find out.”
Vanderbilt is one of a few U.S. centers with the combined expertise in gynecologic oncology and HIPEC to now be investigating its use. Concurrently, Crispens is helping lead a national NRG Oncology group evaluating approaches for U.S. trials. The group is in discussion with the National Cancer Institute about funding an investigational protocol to include safety, efficacy and the mechanism by which HIPEC may work to eradicate residual cancer cells.
The Dutch Study
Van Driel et al. ran a multicenter, phase 3, randomized controlled trial including 245 patients with stage 3 ovarian, fallopian tube or peritoneal cancer. Prior to surgery, patients received three cycles of neoadjuvant chemotherapy with carboplatin and paclitaxel. If their tumor could be debulked to ≤10 mm threshold, patients received HIPEC using cisplatin (122 patients in total). The remaining 123 patients underwent cytoreductive surgery without HIPEC. All received three more cycles of carboplatin and paclitaxel post-surgery.
Patients who received HIPEC fared considerably better than the control group in recurrence-free survival (14.2 versus 10.7 months), median overall survival (45.7 months versus 33.9 months), and survival at 4.7 years (62 percent versus 50 percent).
“Their findings are encouraging and pave the way for a multitude of studies,” Crispens said. “However, we can’t draw sweeping conclusions from early studies that have narrow criteria, looking at very specific patient profiles. Aggressive cytoreductive surgery with HIPEC is a potentially toxic therapy and may not be appropriate for every patient.” Crispens also emphasized that patients in the Dutch study did not receive concomitant treatments that may affect outcomes.
HIPEC and Limits of Current Therapies
“The greatest immediate appeal of HIPEC… may be as an effective mechanism to finally eradicate residual cancer cells.”
Current treatment of advanced ovarian cancer is neither straightforward nor uniform—specialists vary in their choice of chemotherapy drugs and numbers of cycles, and the decision to administer neoadjuvant therapy. While intravenous chemotherapy administration is more the rule and intraperitoneal the exception, combinations are sometimes used.
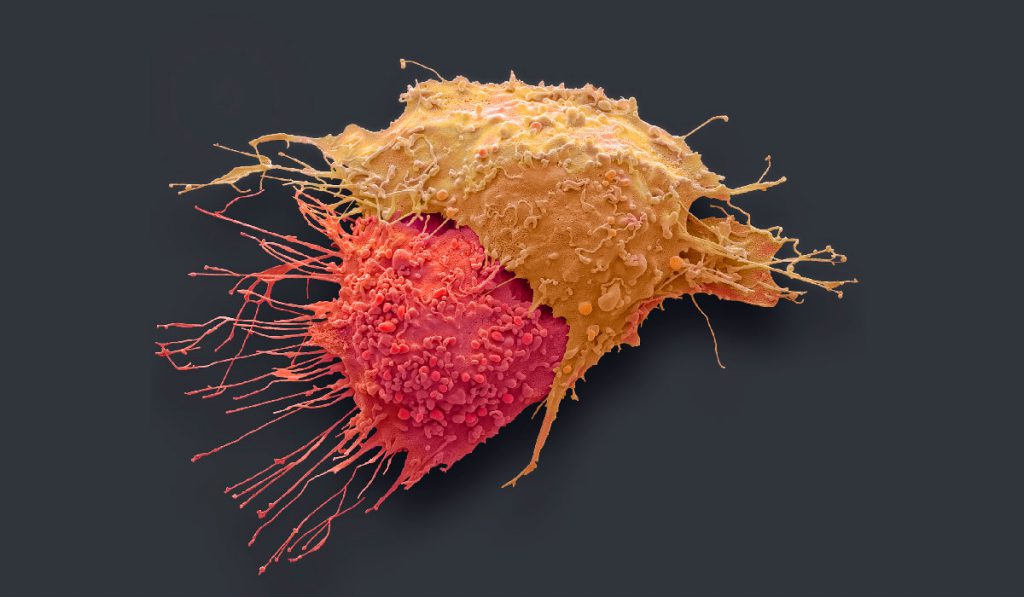
Treatment advances have inched patient survival upward but have not significantly impacted cure rates. “We’re not getting to that stem cell population,” Crispens said. “Even when we debulk to under a centimeter, residual cancer cells are sticking behind and those stem cells eventually are reactivating, dividing and causing a recurrence.”
“The greatest immediate appeal of HIPEC, then, may be as an effective mechanism to finally eradicate residual cancer cells,” Crispens said.
Next Steps
In 2018, on the heels of the Dutch study, a multidisciplinary team at Vanderbilt performed their first ovarian HIPEC procedure. “The results of the van Driel trial provided level 1 evidence that HIPEC has benefits for selected patients with ovarian cancer,” said Kamran Idrees, M.D., a HIPEC specialist and director of the Peritoneal Surface Malignancy Program at Vanderbilt-Ingram Cancer Center. “We want to be instrumental in further validating the procedure within the North American population.”
As U.S. trials develop, Crispens is particularly interested in testing just the singular role the thermic effect has in HIPEC’s efficacy. “We’ve all read about isolated cases where a patient has a febrile response to a pathogen like a bad flu virus, and that winds up eradicating their cancer,” Crispens said. “We can test this by comparing outcomes for patients given HIPEC (with Cisplatin) versus heated saline. If the operative factor is the heated fluid, future patients may benefit from hyperthermic intraperitoneal therapy with reduced side effects.”
Future studies also need to address how other chemotherapy drugs integrate with HIPEC. “There are additional interactions to study,” Crispens said. “Some studies, like the GOG252 trial, are showing that when bevacizumab is added to intraperitoneal therapy, the benefit to the patient is lost.”
The Dutch study did not stratify patients by BRCA status, but results from the SOLO-1 trial suggest it is important. “Poly ADO ribose polymerase inhibitors (PARPis) like olaparib, are demonstrating excellent results as maintenance therapy drugs for patients with BRCA1 or BRCA2 mutation, and should also be studied when integrated with HIPEC,” Crispens said.