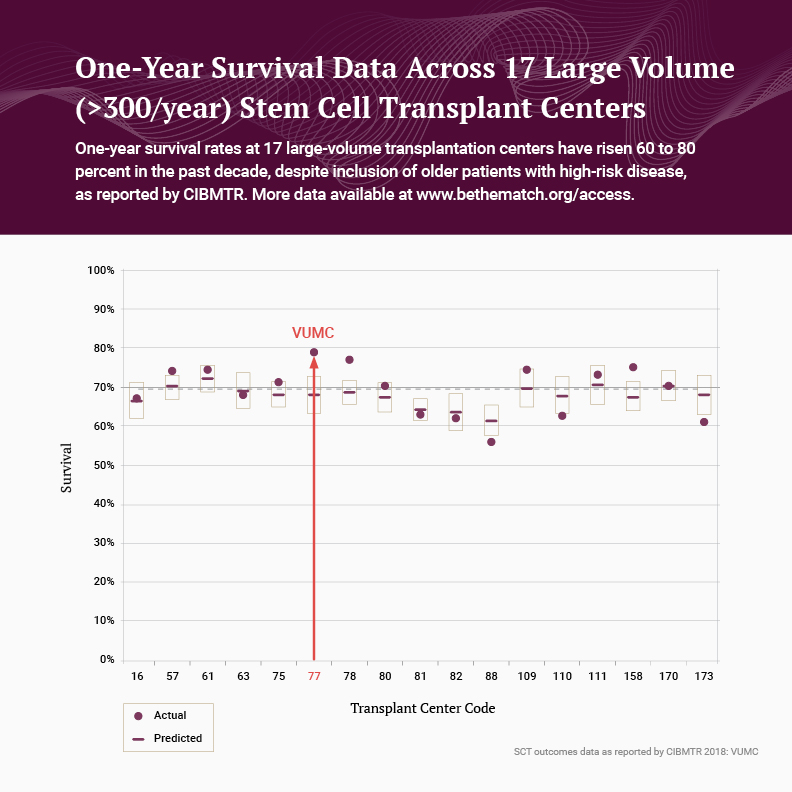
“Allogeneic stem cell transplantation is now a safer option than ever before,” says Bipin Savani, M.D., director of the Long-Term Transplant Clinic at Vanderbilt University Medical Center. Vanderbilt ranks among the best in the nation for donor stem cell transplant survival rates, yet Savani points to a trend toward still better outcomes. One-year survival rates have risen 60 to 80 percent over the past decade despite inclusion of older patients with high-risk disease.
As good as this news is, patients who cross the two-year survival milestone are rarely free of ongoing concerns about recurrence or other morbidities. To help improve long-term outcomes in survivorship, leading medical centers are turning attention to new programs and strategies, Savani says.
“Once we could get a high percentage of patients through the first 100 days, the first year, and then the first two years, the question became how to give them a life span approaching that of the general population, and how to optimize their quality of life.”
Refining the Allogeneic HCT Procedure
In allogeneic hematopoietic cell transplantation (HCT), a donor’s hematopoietic cells are infused into the recipient’s bloodstream to replace malignant bone marrow cells. Patients undergo chemotherapy, with or without radiation, to deplete their own marrow stem cells and create a space for transplanted cells. The most common indications for allogeneic HCT in adults are acute myeloid leukemia and myelodysplastic syndrome.
In contrast to multiple myeloma and lymphoma patients, who commonly undergo an autologous peripheral blood stem cell graft, allogeneic HCT patients need a hematopoietic cell source (i.e., stem cell donor). “A first degree relative who is a good match is ideal,” said Savani. “But because transplantation is the only viable option for many of these patients, we also use cells from matched or mismatched unrelated donors.”
Patients use immunosuppressive medications to minimize rejection and systemic reactions collectively known as graft-versus-host disease (GVHD). They also stay near their transplant center for several months for check-ups and rapid access to care. “In the first three months, risks are particularly high, so we closely watch for disease recurrence, GVHD and infection,” Savani said.
Reducing Long-term Risks
The leading cause of death in long-term survivors is a malignancy — either cancer recurrence or a secondary malignancy due to immunosuppression, a viral reactivation or the intensity of the chemotherapy and radiation.
The second leading cause of death is chronic GVHD, which can compromise the lungs, eyes, kidneys, liver and other organs. GVHD affects 30-50 percent of allogeneic recipients, Savani said. “Patients on long-term immunosuppressive therapy for chronic GVHD also have an elevated stroke risk and an incidence of heart attack seven-fold that of the general population.” Acute infection also presents an ongoing risk to HCT patients.
Stem cell transplant centers are taking innovative approaches to these threats. Vanderbilt has developed a two-pronged strategy, beginning with an intensive long-term follow-up program, involving return visits for examinations and lab tests, disease screenings, drug level monitoring and an aggressive immunization regimen to minimize infection risks.
The second component involves new tools for pre-emptively attacking the roots of morbidities. “The biggest factor in long-term survival rates is the improved and refined management of chronic GVHD,” Savani said. Incorporating new steroid-sparing drugs in both pre-transplantation conditioning and ongoing care can reduce immunosuppression side effects and the risks of GVHD. Extracorporeal photopheresis is another therapy now used for its steroid-sparing effects, improving quality of life in patients with chronic GVHD.
Seeing the Effects
“In the past, if you had a lot of comorbidities, we didn’t do the transplant… That is no longer a big barrier for us.”
The payoff at Vanderbilt is a long-term survival rate of 80 percent. “We have also extended our reach, more than doubling the number of transplant procedures between 2000 and 2016,” Savani said.
Not only are patients living longer, but allogeneic HCT, once offered only to patients under 60, is now offered to patients up to 75 years old. “In the past, if you had a lot of comorbidities, we didn’t do the transplant because of the high risk of procedure-related mortality,” Savani said. “That is no longer a big barrier for us. We do it for every patient possible because it’s their only option to stay alive.”