A major complication of advanced chronic kidney disease (CKD) and end-stage renal disease (ESRD) is anemia. This is primarily due to the diminished ability of diseased kidneys to produce adequate amounts of erythropoietin (EPO), the glycoprotein hormone that is essential for normal erythropoiesis. Hypoxia-inducible factor (HIF), an oxygen-sensitive transcription factor that helps cells survive hypoxic environments, induces the synthesis of EPO. The kidney is the primary EPO production site in adults, but the liver also has the capacity to synthesize EPO when appropriately stimulated (see review in Nature Reviews Nephrology).
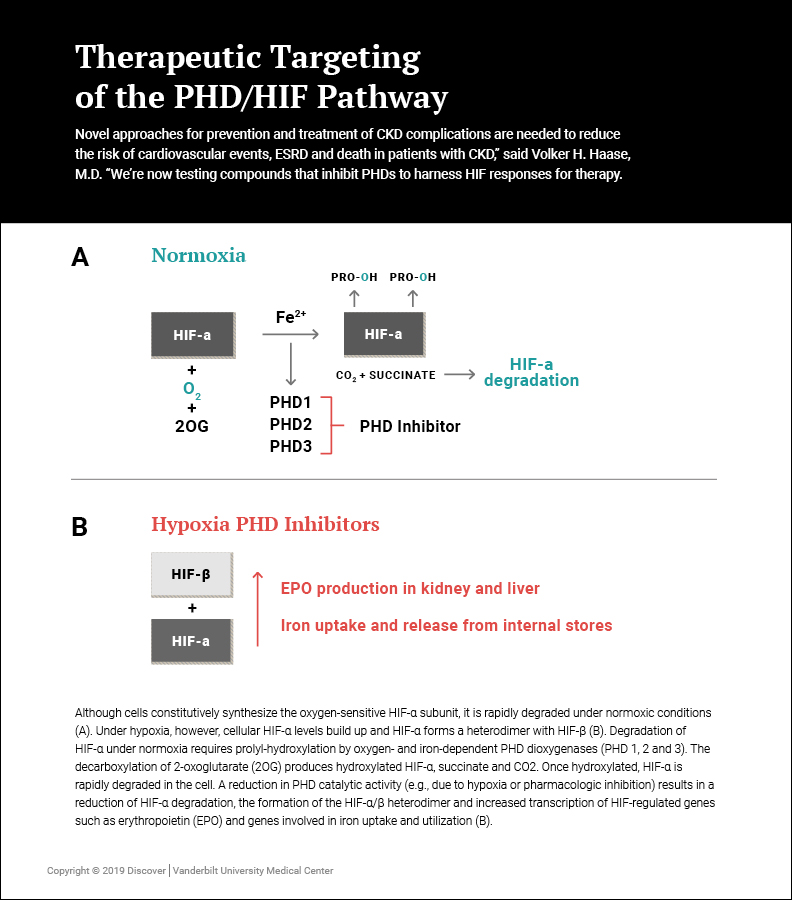
HIF responses are controlled by prolyl hydroxylase domain (PHD) oxygen sensors, which regulate a broad spectrum of cellular functions. The discovery of PHDs has led to the development of novel drug compounds that reversibly inhibit PHD catalytic function, activate HIF responses and stimulate the endogenous production of EPO, which holds enormous promise for anemia therapy.
“Novel approaches for prevention and treatment of CKD complications are needed to reduce the risk of cardiovascular events, ESRD and death in patients with CKD,” said Volker H. Haase, M.D., the Krick-Brooks Chair in Nephrology at Vanderbilt University Medical Center. “We’re now testing compounds that inhibit PHDs to harness HIF responses for therapy.”
A 2017 paper published in Hemodialysis International provides a concise overview of the clinical effects associated with pharmacologic PHD inhibition in CKD and ESRD patients.
The PHD/HIF Axis in EPO Regulation and Iron Metabolism
Haase studies the molecular links between oxygen sensing, renal metabolism and CKD. His laboratory uses conditional gene targeting technology as well as biochemical and functional genomics approaches to define the specific roles of HIF transcription factors in CKD and its complications, such as anemia and iron deficiency. In 2007, using a mouse model, Haase’s laboratory identified HIF-1 as the first molecular link between hypoxia and CKD progression.
In a 2012 study, Haase and co-investigators used a genetic mouse model to dissect the role of HIF in the regulation of hepcidin, a small peptide that controls the amount of iron available for the production of new red blood cells. “Iron uptake is often a problem with these patients,” Haase explained. “In patients with advanced CKD, plasma hepcidin levels are frequently elevated and contribute to the development of anemia as increased hepcidin leads to functional iron deficiency.”
The investigators reported that HIF suppresses hepcidin indirectly, by stimulating EPO-induced erythropoiesis, as EPO itself did not directly regulate hepcidin levels. The findings promoted better understanding of targeted therapies aiming to exploit the HIF oxygen-sensing pathway for treating anemia and disorders of iron balance.
Developing New Therapies for Renal Anemia
Several compounds for the treatment of renal anemia are now in phase 2 and phase 3 clinical trials. “For years, we’ve been giving a recombinant form of EPO to patients,” said Haase, “but sometimes patients need a very high amount of EPO to get a response, which increases the risk of cardiovascular side effects such as stroke and myocardial infarction. These new drugs offer another way of treating anemia by stimulating the production of EPO in the kidneys and liver, and by improving iron metabolism.”
“Because of its dual action on EPO and iron homeostasis, pharmacologic targeting of the HIF oxygen-sensing pathway has become a very attractive approach for the treatment of anemia,” he said. “We expect that the FDA will approve some of these compounds. There haven’t been that many new drugs for renal patients in years, so this will be a big change for patients with CKD.”