Gastrointestinal reflux disease (GERD) affects a fifth of the U.S. adult population, but it remains challenging to diagnose due to high symptom overlap with non-GERD conditions (such as eosinophilic esophagitis, EoE) and the burden of prolonged ambulatory monitoring, which can discourage many patients.
A novel diagnostic tool could resolve those problems, says Michael Vaezi, M.D., director of the Center for Swallowing and Esophageal Disorders at Vanderbilt University Medical Center. Vaezi and colleagues invented a technology compatible with standard endoscopy that directly measures mucosal impedance (MI) and recognizes the unique epithelial signature of GERD and other esophageal conditions.
The MiVuTM system is the first of its kind to receive FDA approval. ”We expect direct MI testing to greatly improve the practice of how GERD and other esophageal diseases are diagnosed,” Vaezi said.
”We expect direct MI testing to greatly improve the practice of how GERD and other esophageal diseases are diagnosed.”
”The aim of this technology is to provide point-of-care testing during endoscopy and provide an instant diagnosis, which patients really appreciate,” added Dhyanesh Patel, M.D., a gastroenterologist at Vanderbilt and member of the research team.
GERD Diagnosis with Direct MI
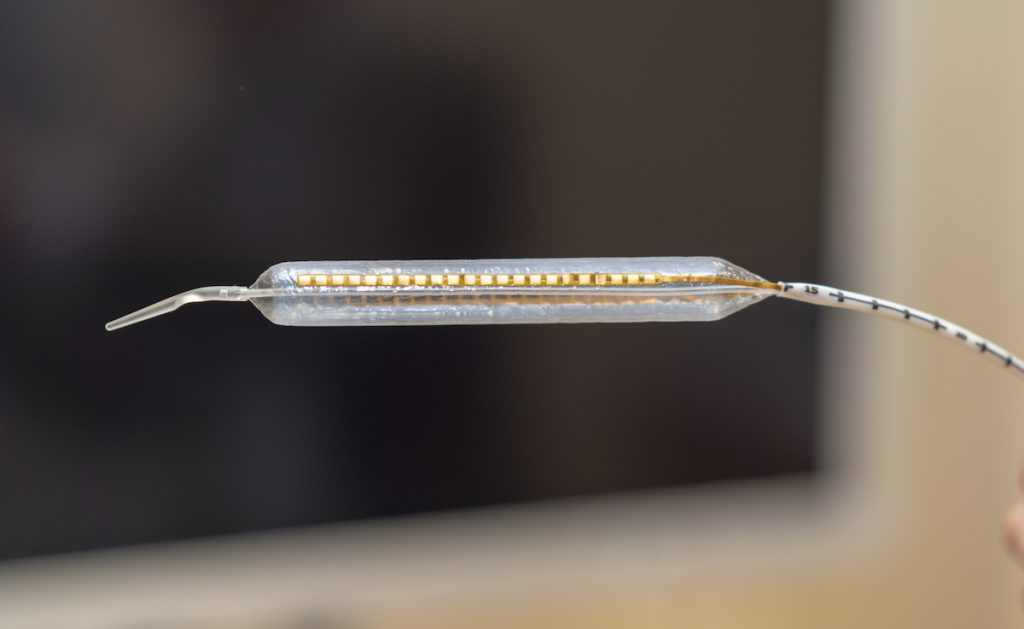
Unlike older diagnostics, the direct MI approach identifies a unique signature of change in the esophageal lining caused by reflux. Using a novel probe placed through the working channel of the endoscope, mucosal conductivity is measured directly through surface contact.
“These signatures – as we call them – are unique,” Vaezi explained. “With GERD, the lining of the esophagus alters in a different way than with EoE. Because each signature is different, we can also look for other diagnoses like gastroparesis that may mimic symptoms of GERD.”
The direct MI evaluation offers diagnostic specificity, Vaezi said. “Instead of inserting a catheter in the nose that just measures acidity or esophageal exposure to acidity, we have a direct view of changes in the lining of the esophagus we can associate with a specific chronic condition like reflux.”
Vanderbilt has conducted several studies showing effectiveness of the direct MI technology for diagnosing GERD versus EoE and other esophageal conditions, and for GERD diagnosis in patients with extraesophageal symptoms. One study in patients with EoE showed that direct MI evaluation could be used to measure treatment response.
”The aim of this technology is to provide point of care testing during endoscopy and provide an instant diagnosis.”

Advantages for Patients
“Our system is much more comfortable for patients than the older diagnostics,” Patel said. It eliminates the need to wear a nasal catheter for long periods of time or undergo a biopsy. “Results are fast, too. We give the patient a diagnosis immediately, not after 24 to 48 hours,” he said.
Work to improve the device is ongoing through multicenter studies which promise to make the model much more robust, Patel said. For instance, the initial research did not define what completely normal mucosa looks like. “We need to know this so the model will get better at predicting deviations from the norm,” he said.
“Our system is much more comfortable for patients than the older diagnostics.”
Efforts are also underway to teach the model to factor in clinical parameters that a human diagnostician would immediately consider, Patel said. “When I see a 36-year-old male with dysphagia, I immediately think eosinophilic esophagitis. The machine can improve by learning to factor in key clinical features as well.”