Up to 67 percent of physicians in the U.S. report symptoms of burnout – including emotional exhaustion, depersonalization and a low sense of personal accomplishment. Burnout rates are rising, and front-line specialties (emergency medicine, internal medicine and family medicine) are often hit hardest.
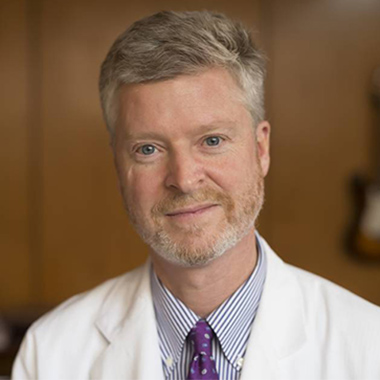
“There is a recognition nationally that there is a problem in medicine,” says Reid Thompson, M.D., William F. Meacham Professor and Chair of Neurological Surgery at Vanderbilt University Medical Center. “Whether burnout is a new problem is not clear, but what is clear is that it seems to be on the upswing.”
In 2011, the Mayo Clinic and American Medical Association (AMA) collaborated on the first large-scale study of physician burnout in the U.S., using the Maslach Burnout Inventory (MBI) questionnaire. Many subsequent studies, including an update to the Mayo Clinic-AMA survey in 2014, corroborate that physician burnout is widespread across practice settings.
Creating a Task Force for Empowerment and Well-being
Recognizing that physician burnout is becoming a critical issue for all healthcare systems, Vanderbilt launched the VUMC Task Force for Empowerment and Well-being in 2017. The task force, which is co-chaired by Thompson and Executive Director of Faculty and Staff Health and Wellness Mary Yarbrough, M.D., includes 14 additional members from across the adult hospital and Monroe Carell Jr. Children’s Hospital at Vanderbilt.
“Vanderbilt had invested early in this issue, establishing one of the first faculty health and wellness programs in the country,” said Yarbrough. “We knew it was time to leverage those current resources and advance further. We created the task force to understand our specific situation at Vanderbilt – what do our physicians need to feel empowered, confident and supported?”
The task force began with a two-question survey of all Vanderbilt physicians:
- What do you need to do your best work and enhance your personal well-being?
- If 10 reflects your optimal health and wellness and 0 reflects burnout or significant professional stressors or concerns, where do you place yourself on this scale?
About half of Vanderbilt physicians rated themselves below 5 on the wellness scale. But their answers to the first question revealed opportunities, with large proportions of the 1,064 respondents mentioning self-care (41 percent), leadership support (34 percent), and staffing support (28 percent) as ways to enhance their well-being.
“Of the areas identified at our institution for improvement, the three themes that resonated the most with our Vanderbilt physicians included autonomy, efficiency and community,” says Cristina Estrada, M.D., associate professor of Clinical Pediatrics and the Division Chief of Pediatric Emergency Medicine.
From the survey data, the task force extracted a number of “first-order” interventions to provide immediate relief to physicians in the adult and children’s hospitals. These immediate measures included more encouragement to physicians to see their own doctors, adjustments to childcare hours, EHR support and improved parking for all shifts.

Changing Hospital Culture for the Long Term
The task force is planning changes far beyond the immediate recommendations, says Yarbrough. The group’s emphasis is proactive, focused on forward-thinking improvements to Vanderbilt’s hospital culture. “We chose the name Task Force for Empowerment and Well-being purposefully, to avoid the term ‘burnout,’” Yarbrough said. “Our focus is on moving toward a preventive state, making long-term improvements that will benefit all clinicians, as well as physicians.”
The task force’s plan is tiered. After the first-order interventions are complete, the group will advance to interventions that have a longer implementation cycle, are considered more difficult or complex or that require more budget or resources.
Second-order interventions may include more permanent structures encouraging physicians to attend to personal health and self-care, and to their families’ care; an Office of Physician Well-being; more exercise options in the workplace; and more intentional discussions of well-being and meaningful work as part of employee onboarding and ongoing career planning. Educational opportunities, such as retreats, are also planned to equip physician leaders with strategies to discuss well-being with staff.
Establishing Accountability
The task force is currently meeting with department chairs to share enterprise- and department-level survey results. Together, they will identify “department wellness champions” to facilitate support within work units. “We know that you can change the culture if you start talking about well-being, thinking about it, modeling it, and holding people accountable,” Thompson said.
The task force recommends that a standard measure of well-being be used at the department level to assess retention and intervention progress. Faculty retention rates and use of wellness and health promotion facilities will also be incorporated into long-term wellness monitoring. The goal is to ensure that every Vanderbilt physician, clinician and staff member across the medical center community is included in wellness improvements.
“We are fortunate to be part of an institution that is invested in this important work and is committed to leading change nationally,” said Estrada.