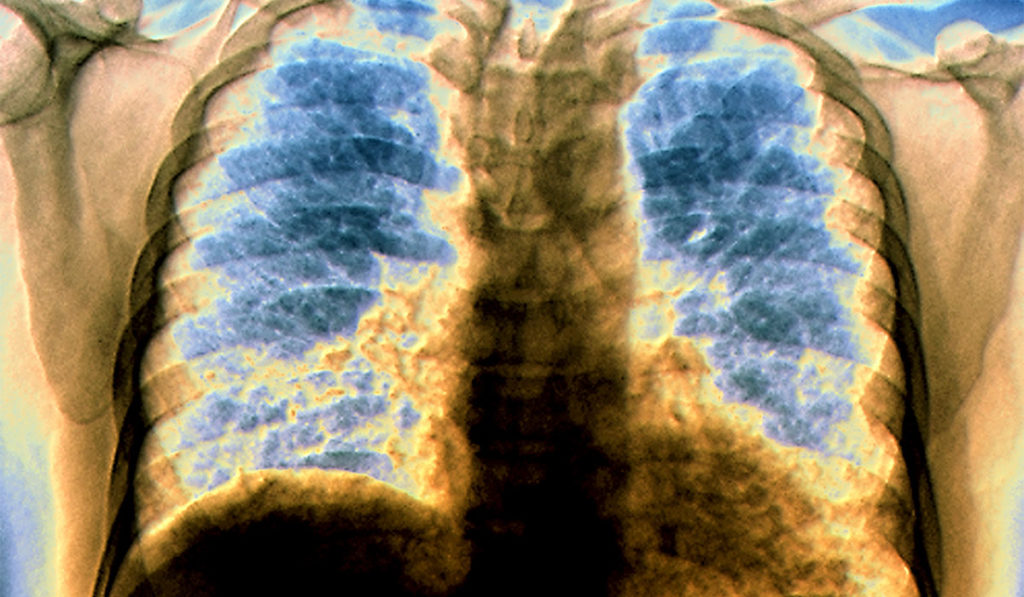
Recent leaps in understanding how the immune response drives lung fibrosis may soon lead to an effective treatment for pulmonary sarcoidosis. Fibrosis is the leading cause of death in the 30 to 40 percent of sarcoidosis cases that progress to a chronic condition.
Today, anti-inflammatory treatment (Prednisone) remains the current standard of care for severe pulmonary sarcoidosis. Until the past few years, disease progression has been nearly impossible to predict.
“Right now, we’re using medicines that amend the immune system so patients have less symptoms. In the majority of patients, when we stop the medications, the disease comes back,” said Wonder Drake, M.D., the director of the Sarcoidosis Center of Excellence at Vanderbilt University Medical Center. Drake’s research over the past decade has led the sarcoidosis community to recognize the foundational role of the immune system in promoting or inhibiting chronic sarcoid progression. Now, this research is pointing to new potential therapies.
Identifying Immunologic Drivers of Disease Progression
Drake’s research team published a key study in 2013 identifying the role of CD4+ T cell immune function in sarcoidosis clinical outcome. A second study, published in 2014, showed increased expression of the programmed death-1 protein (PD-1) on sarcoidosis CD4+ T cells was a key driver of the observed loss of immune function.
The most recent study from Drake’s group, published in 2018 in Science and Translation Medicine, suggests inhibiting PD-1 uptake in TH17 cells may be an effective therapy to prevent fibrosis in pulmonary sarcoid cases. By blocking the PD-1 pathway in CD4 + cells using antibody against PD-L1, or the small-molecule inhibitor of a key transcription factor STAT3 (STATTIC), the study showed significant declines in collagen-1 production and concomitant fibrosis development.
“We had already established that immune system strength is an important factor in re-solving sarcoidosis,” Drake said. “We had also showed that increased expression of PD-1+CD4+ T cells was highest in sarcoidosis subjects experiencing progression of their pulmonary sarcoidosis and the lowest in subjects who were resolving their disease. Now, by inhibiting PD-1, we have been able to significantly reduce pulmonary fibrosis in mouse models.”
The most recent study included immunohistochemistry analysis of patient cohorts from Vanderbilt, Cleveland Clinic, and the University of Cincinnati, including patients with active sarcoidosis, resolved disease, idiopathic pulmonary fibrosis (IPF), and healthy controls. The study required extensive collaboration, with thirty authors credited from around the globe. Immunohistochemistry revealed increased PD-L1 expression within sarcoidosis granulomas, as well as PD-1 upregulation on IPF CD4+ T cells. Patients with sarcoidosis and IPF were shown to have programmed death-1+ (PD-1+) CD4+ T cells with reduced proliferative capacity and increased TGF-ß/IL-17A expression. The mouse component of the study employed bleomycin-induced pulmonary fibrosis to show PD-1 path-way blockade using antibody against PD-L1 significantly inhibited collagen-1 production and reduced fibrosis.
Next Steps
Drake is encouraged by the prospect that new, autoimmune-directed therapies for pulmonary sarcoidosis will leverage existing, FDA-approved drugs. “All of the therapeutics we’ve identified currently are FDA approved. That’s a boon right there. If we can show these medicines work in rigorous clinical trials, we’ve bypassed many of the regulatory processes required to move new treatments forward.”
“All of the therapeutics we’ve identified currently are FDA approved. That’s a boon right there. If we can show these medicines work in rigorous clinical trials, we’ve bypassed many of the regulatory processes required to move new treatments forward.”
Drake sees growing national, and even international, research collaboration as a catalyst for even more rapid advances in sarcoidosis treatment and prevention. As one example, Vanderbilt is currently participating in a six-center phase II trial of oral antimycobacterial therapy for progressive pulmonary sarcoidosis using the CLEAR (Combination Levofloxacin, Ethambutol, Azithromycin, and Rifampin) treatment regimen.
“I realized early in my own research that the people investigating sarcoidosis are brilliant. Yet we weren’t making a big enough dent in the disease,” said Drake. “Everybody needed to push in the same direction at the same time, using our diverse skills.”
“Now, we’re making real progress,” said Drake. “I am actually quite hopeful that we’re going to cure this disease.”