In the United States alone, more than one million people live with lower limb loss or difference, and this number is only expected to increase. Lower limb prosthesis users often exhibit enduring gait asymmetries, with variably executed walking performance that can lead to functionally debilitating impairments (secondary degeneration). Observational gait analysis, which relies on subjective visual assessment, is most often used in the clinical setting to evaluate walking performance.
“There is a pressing need for objective measurement tools that can monitor walking performance in lower limb prosthesis users and in other conditions affecting the walking function,” said Gerasimos (Makis) Bastas, M.D., Ph.D., director of limb loss rehabilitation at Vanderbilt University Medical Center. “We want to intervene before people suffer any adverse events such as falls, injury to the residual limb or further debility through deterioration in the sound limb and elsewhere in the body.”
Advances in Prosthetics
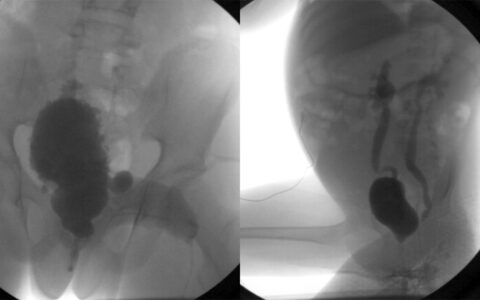
Bastas and colleagues in Vanderbilt’s Mechanical Engineering department are working to develop tools to objectively monitor walking performance in lower limb prosthesis users. One promising tool, an inertial measurement unit (IMU, an accelerometer), is being leveraged to identify the asymmetries and consistency exhibited by patients during walking. The accelerometer, mounted on the pelvis, measures discrepancies in the movement afforded by sound versus prosthetic limb and employs novel, sophisticated step demarcation algorithms to estimate changes in gait.
“Every patient’s gait is asymmetrical, but uniquely theirs,” Bastas said. “With this tool, we can establish a baseline walking signature and track it over time, sensitively noting when something is changing early on—perhaps in the prosthetic fit, alignment or comfort or the patient’s intrinsic ability to walk. Such a tool may permit us to intervene timely to stave off further deterioration.”
Functional Assessment of Prosthetics
At the American Congress of Rehabilitation Medicine Conference last October, Bastas delivered a symposium on the “Medical Considerations for Prosthetic Candidacy, Enduring Functional Enablement and Coordination of Care.”
“There’s a difference between prosthetic performance and enablement,” Bastas explained. “We focus on enablement. Limb loss or difference can affect the entire life span. We’re developing a continuum of care that takes stock of patients’ particular needs, abilities and overall state of health, and tends to them in a truly interdisciplinary fashion to help them meaningfully self-actualize in their personal, vocational and recreational endeavors.”
“Every patient’s gait is asymmetrical, but uniquely theirs. With this tool, we can establish a baseline walking signature and track it over time, sensitively noting when something is changing early on.”
Vanderbilt’s limb restoration care clinic employs this interdisciplinary approach, with a focus on improving clinical approaches to better patients’ outcomes and quality of life. Physiatrists evaluate factors that may impact overall energy. Clinicians provide consultative support for surgical colleagues, work closely with physical and occupational therapists, and collaborate with prosthetists. Education and psychological support are key elements.
“Whether it’s a congenital limb absence or an amputation later in life, patients need individualized and contextualized education, not just information,” Bastas said, “as well as resources and logistical and psychological support. Most of these patients find themselves having to renegotiate life anew—everything from performing basic functions and tasks to negotiating new realities about themselves, their expectations and those of others. We take the journey with them. We want them to have the best possible quality of life.”
Development of National Guidelines
Bastas is a founding member and the inaugural chair of the Limb Restoration Rehabilitation Group (LRRG), an international interdisciplinary group aiming to promote research endeavors, clinical care delivery and overall enablement outcomes for people with limb restoration needs. The LRRG is a content-specific interest group within American Congress of Rehabilitation Medicine.
“There are certainly a lot of areas where we can stand to grow our collective fund of knowledge surrounding the medical care of the limb loss or difference patient, to finally bolster practice guidelines surrounding limb restoration health and enablement,” Bastas said. “The big battle we face is making sure our patients have access to the resources, prosthetic technologies and health-related services they need.”
The group hopes to create professional networks, initiate multi-site trials and establish registries. “This is about how we value our patients,” Bastas said. “We want this to be a rallying group for true improvement in the field.”