Recent studies employing brain lesion mapping have provided insight into how lesions may be connected to neurologic symptom generation for conditions including hallucinations, involuntary movements, delusions and loss of consciousness. Brain lesion mapping is the identification of heterogeneous brain regions functionally connected to a lesion location.
New research into patients with spatially diverse lesion locations and lesion-induced criminal behavior, or “acquired sociopathy,” suggests a connection between this behavioral phenotype and a common functional brain network linked to morality. The research, published in the Proceedings of the National Academy of Sciences was conducted by Ryan Darby, M.D., Vanderbilt University Medical Center; Andreas Horn, M.D., Ph.D., Beth Israel Deaconess Medical Center; Fiery Cushman, Ph.D., Harvard University; and Michael D. Fox, M.D., Ph.D., Beth Israel Deaconess Medical Center.
Mapping Lesions Associated with Criminal Behavior
“The idea that brain networks are important for cognition has really become popular in the last 10 to 15 years,” said Darby, assistant professor of neurology at Vanderbilt. “A lot of that has been the result of looking at resting state functional connectivity. That approach hasn’t been applied as much to specific syndromes in neurology, especially lesion syndromes where the lesions occur in different areas. Our research is the first applying that approach of using connectivity as a map to analyze lesions to study criminal behavior.”
The main study examined published case records and brain lesion images of 17 individuals with known lesion-induced criminal behaviors, including violent and nonviolent crimes. Lesion location varied across cases, including lesions in the medial frontal or orbito-frontal structures (nine individuals), medial temporal lobe/amygdala (three individuals), anterior lateral temporal lobe (three individuals), dorsomedial prefrontal cortex (one individual) and ventral striatum and parts of the orbitofrontal cortex (one individual).
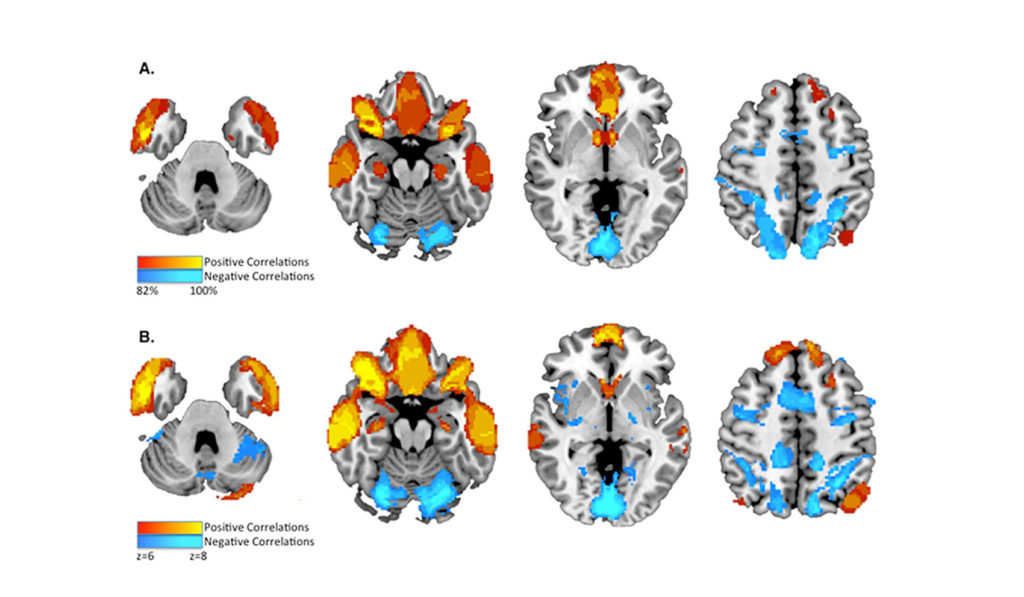
Employing brain lesion mapping using a database of functional state resting connectivity from normal subjects, the study showed that all or most of the 17 individuals with acquired sociopathy had lesion sites positively correlated to the inferior orbitofrontal cortex and anterior temporal lobes (17 individuals) and the ventromedial prefrontal cortex (vmPFC) and nucleus accumbens (16 individuals). In addition, most or all lesion sites were negatively correlated with the intraparietal sulcus (17 individuals) and dorsolateral prefrontal cortex (15 individuals). Further analysis of 23 cases of individuals with criminal behaviors and lesions of unknown temporal relationship showed a nearly identical brain lesion mapping.
Connections to Moral Decision Making
To explore if this network localization of lesions associated with criminal behavior was uniquely functionally connected to brain regions involved in moral decision making, the study employed, in the data-driven engine Neurosynth, meta-analyses of task–fMRI activation studies for the terms “morality,” “value,” “theory of mind,” “empathy” and “cognitive control.” In addition, the study included manually performed meta-analysis of fMRI studies of morality using activation likelihood estimation (ALE).
Results showed that lesions temporally associated with criminal behavior are functionally connected to regions activated by moral decision making, value-based decision making and theory-of-mind tasks. The lesion sites are not connected to regions activated by empathy or cognitive control.
“This network seemed to be the same one involved in moral decision making but not other things that may be important for behavior, like empathy,” Darby said. “We tried to replicate the results in the 23 patients with lesions of unknown temporal association with criminal behaviors. Those results lined up with the same network.”
Implications of the Study
The finding that lesions in criminals, while heterogeneous, do localize to a unique resting state network associated with key subcomponents of moral decision making may open multiple avenues of research.
“We anticipate exploring other neurological diseases in which patients might be more prone to criminal behavior,” Darby said. “In frontal temporal dementia, for instance, somewhere between 40 to 60 percent of patients commit a crime as part of their disease course. These are often nonviolent crimes, things such as theft or indecent exposure. We’d like to understand if the same network is involved, where those regions are atrophied and, if those patients do commit crimes, do they have neurological changes in their value-based decision making or moral decision making.”
Darby advises a cautious approach to interpreting the current study. “A brain lesion in this network does not mean that someone is inevitably going to commit a crime,” he said. “It’s important to note that we selected cases where we knew they had committed a crime. In reality, someone with a frontal lobe injury probably only has a 10 to 15 percent chance of committing a crime. There are clearly other factors besides having a brain lesion that contribute to these criminal behaviors.”
“The question of legal responsibility is also very complex. This and other studies point toward the brain as being important for regulating our behavior to abide by the law, but the presence or absence of a brain injury doesn’t necessarily change whether we as a society decide if someone is responsible or not.
Listen to an audio interview with Ryan Darby, M.D., about new research into brain networks’ role in lesion-induced criminal behavior.