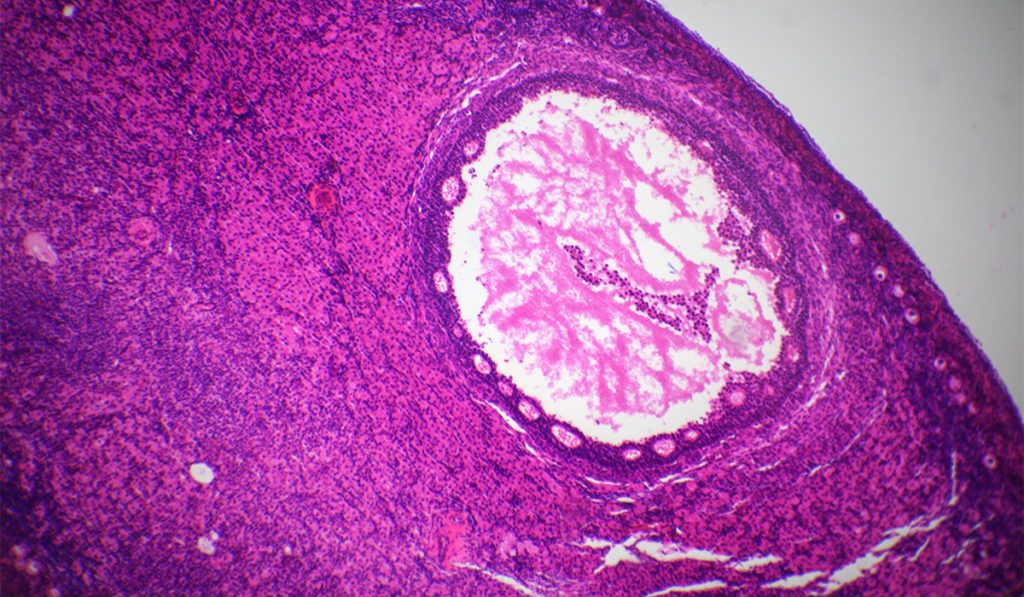
Polycystic ovary syndrome (PCOS) — which affects 5 to 10 percent of women — is characterized by clinical or biochemical evidence of elevated androgens and irregular menstrual cycles. An ultrasound usually reveals multiple ovarian “cysts,” an abundance of immature follicles in which development stopped early due to abnormal ovarian function.
Symptoms and Diagnosis of PCOS
PCOS affects both adolescents and adult women. Typically, women will experience oligomenorrhea (less than nine periods per year or cycles longer than 35 days). Women with PCOS are more likely to be overweight or obese, which can lead to insulin resistance and increased androgens, causing secondary effects like hair growth and acne. Women with PCOS also have an increased risk of developing adult onset diabetes, high blood pressure, high cholesterol and infertility.
Classically, PCOS is characterized by anovulation, leading to unopposed estrogen. Unopposed estrogen can lead to endometrial hyperplasia and, if left untreated, to endometrial cancer. Women with PCOS who are not actively trying to conceive should use hormonal contraception for endometrial protection. Lifestyle changes, such as weight loss, can improve PCOS symptoms. Metformin can be used off-label to treat insulin resistance and, additionally, assists with ovulation.
A variety of less common disorders can present similarly to PCOS. Because of this, it is routine to obtain laboratory tests, and sometimes a urine collection, to exclude other issues. Other causes of menstrual irregularity such as elevated prolactin and thyroid dysfunction should be ruled out.
New Approaches to Treatment
Because PCOS is multisymptomatic, patients often feel isolated and need counseling and support. In consideration of this, a new approach to treating the disorder is being tried at a handful of academic medical centers – comprehensive care clinics devoted solely to PCOS. These clinics are taking a multidisciplinary approach. OB/GYNs and other specialists are working collaboratively to address PCOS symptoms.
“This disorder requires a lot of patient counseling and education. At Vanderbilt, we have all the resources in one place.”
Last summer, Vanderbilt University Medical Center established a PCOS clinic as part of its women’s health program. “We’ve had amazing response since we opened this clinic,” said Michelle Roach, M.D., the clinic’s director . “We’re getting a lot of referrals from the community. The sense I’ve gotten is that many providers are uncomfortable talking with patients about PCOS. This disorder requires a lot of patient counseling and education. At Vanderbilt, we have all the resources in one place.”
In addition to diagnosing and treating PCOS, Roach and her colleagues at Vanderbilt incorporate education and counseling as a key component of their patient care model. “Patients usually think they just have irregular periods,” explained Roach. “When they hear they have PCOS, they’re often unsure what the diagnosis means or what the future holds. The clinic creates a good support system to let patients know they’re not alone.”
Roach’s plans for the clinic in the future include group education and support for PCOS patients. She also hopes to collaborate with researchers at Vanderbilt who are studying the disorder. “We have all these patients in one place,” she said. “We hope to advance research in the field, with the goal of developing comprehensive care and treatment.”